1) HPV DNA testing offers an alternative or complement to traditional Pap smear testing for cervical cancer screening. Molecular techniques like Hybrid Capture can detect HPV infection more sensitively than Pap smears alone.
2) Studies show that HPV testing followed by Pap testing may be up to 98% sensitive for detecting cervical cancer compared to 75% for Pap testing alone. Using HPV testing as a primary screen for women over 30 could help guide patient management.
3) Target amplification techniques like PCR and signal amplification methods like Hybrid Capture are commonly used for HPV DNA testing. These methods allow for high-throughput screening and detection of multiple HPV types with varying cancer risks.


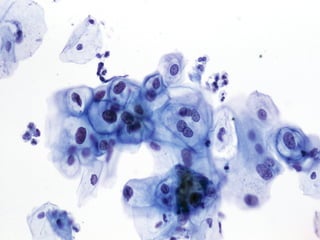






















![DNA test may be more effective than Pap smear for detecting
cervical cancer, studies suggest.
The CBS Evening News (10/17, Couric) reported, "Doctors are telling
us tonight [that] a new test could replace the Pap smear for detecting
cervical cancer."](https://image.slidesharecdn.com/rev4-130907120321-/85/Rev4-hpv-dna-testing-for-s2011-28-320.jpg)