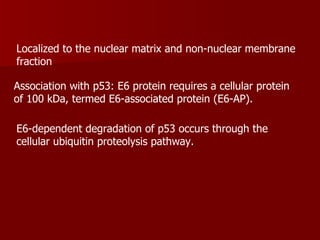
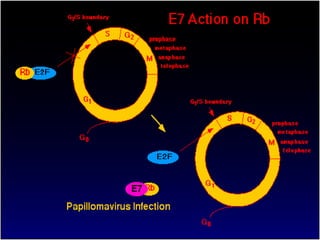
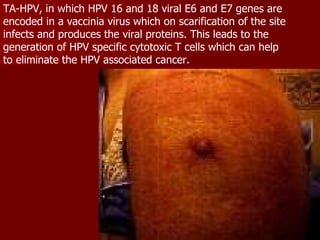
Human papilloma virus (HPV) is a DNA virus that can cause warts and is linked to certain cancers. There are over 100 types of HPV that can infect humans. HPV types 16 and 18 are highly carcinogenic and associated with cervical and other cancers. HPV is transmitted through skin-to-skin contact, usually during sexual activity. While most HPV infections do not cause symptoms and resolve on their own, some types can cause genital warts or warts in the throat. The HPV E6 and E7 proteins contribute to cancer development by degrading tumor suppressor proteins. Vaccines targeting the HPV L1 protein show promise in preventing HPV infection and reducing cancer rates.

























![TREATMENT: Genital Warts TOPICAL CHEMODESTRUCTIVE AGENTS Tri-(or Bi) chloracetic acid (TCA or BCA) Podophyllum: Is an extract of the May apple plant 2. Self Treatments (topical) Condylox[R]: purified podophyllotoxin (podophilox). Imiquimod: an immune response modifier 3. Adjunctive Treatments (no longer extensively used due to side effects (i.e. efudex, interferon)](https://image.slidesharecdn.com/hpv-12638518825143-phpapp02/85/Human-Papiiloma-Virus-28-320.jpg)