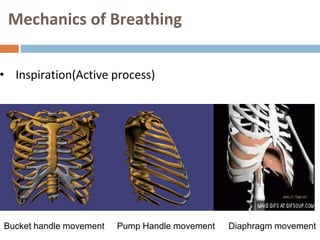
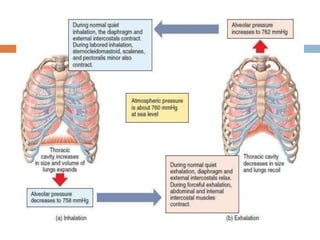
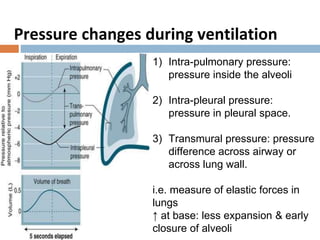
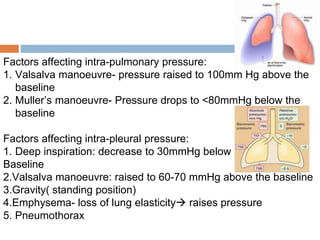
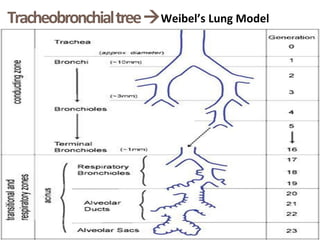
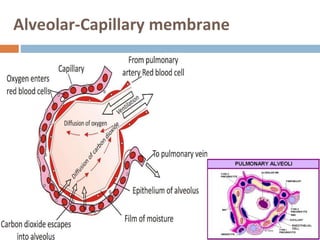
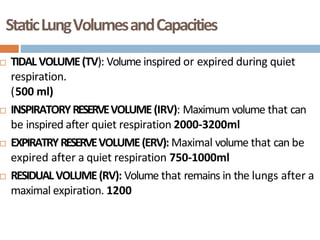
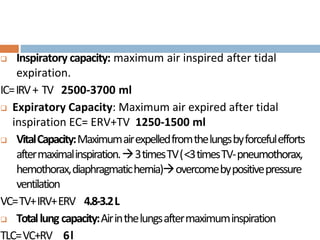
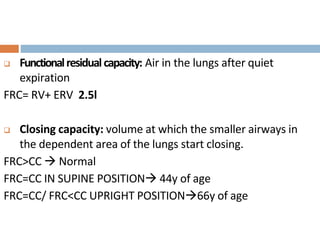
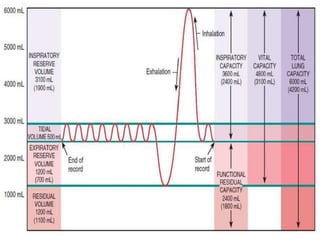
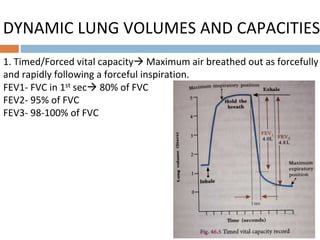
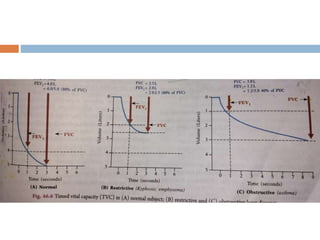
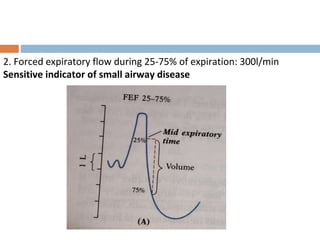
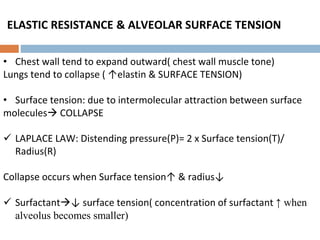
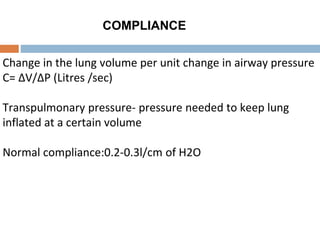
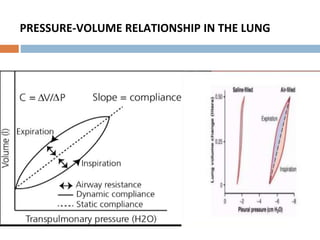
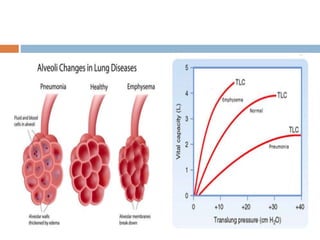
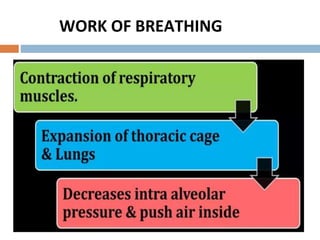
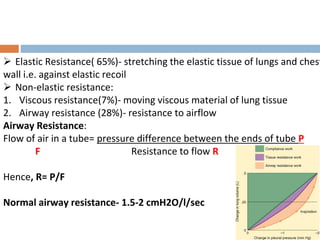
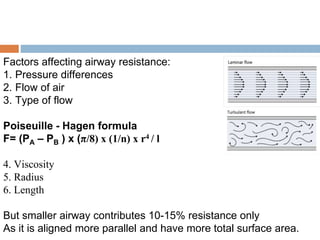
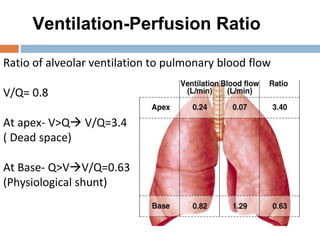
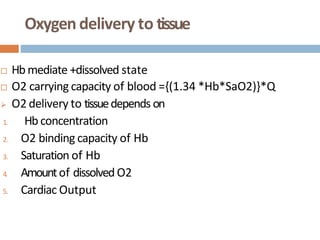
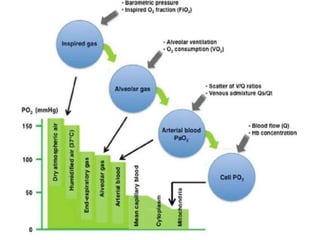
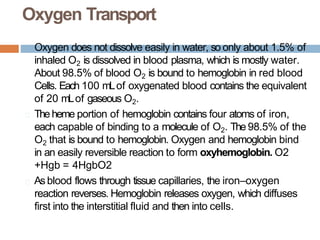
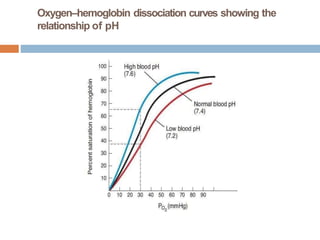
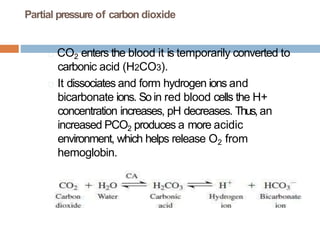
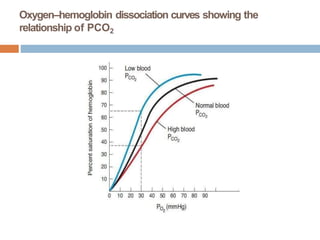
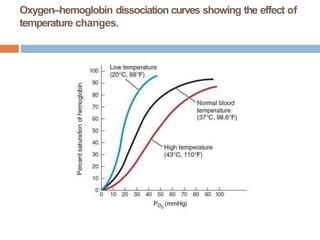
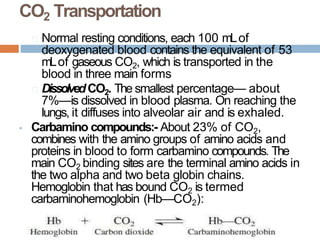
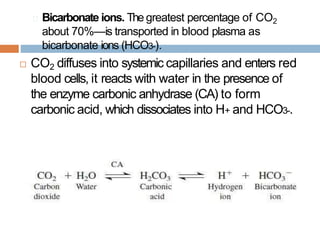
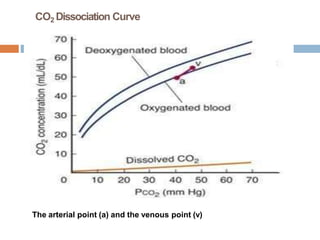
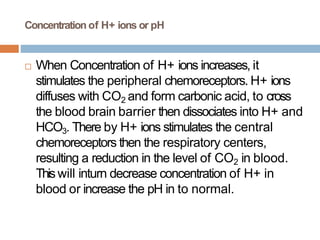
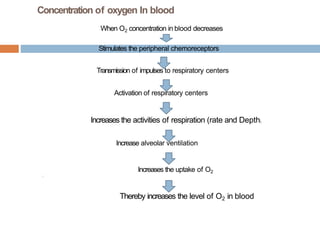
The document outlines key aspects of respiratory physiology, detailing the processes of external and internal respiration, the mechanics of breathing, and the pressures involved in ventilation. It also describes lung volumes and capacities, factors affecting gas exchange, and the oxygen transport mechanisms in the blood. Additional information includes the effects of various factors on hemoglobin and its affinity for oxygen, as well as carbon dioxide transportation in the bloodstream.