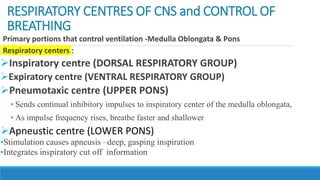
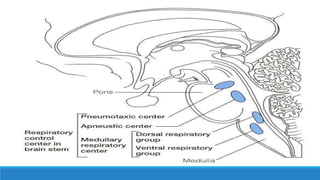
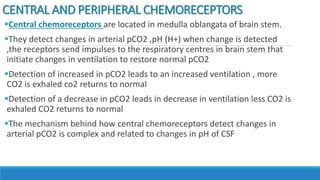
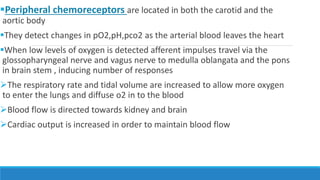
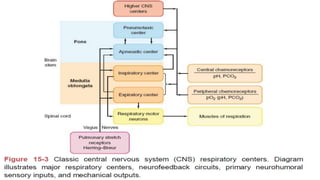
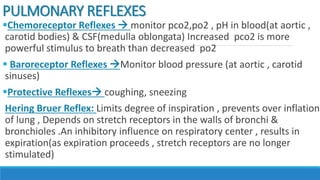
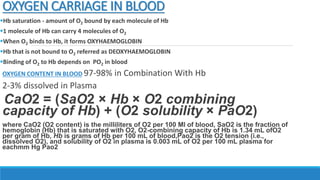
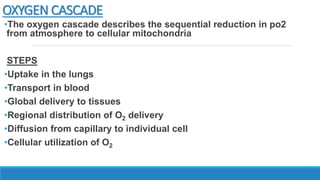
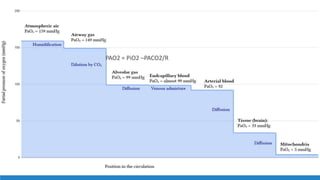
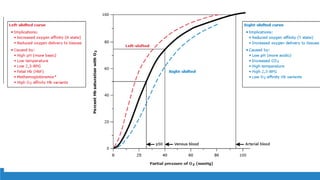
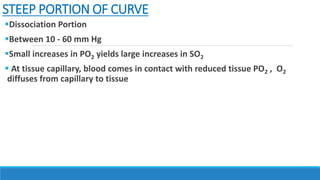
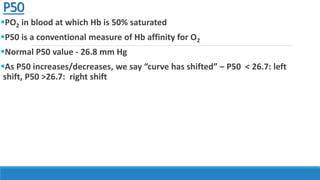
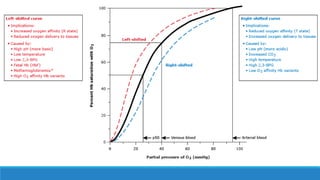
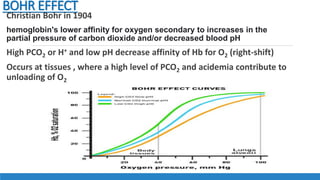
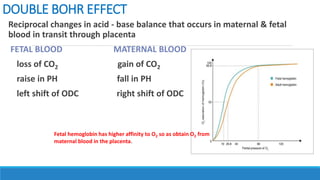
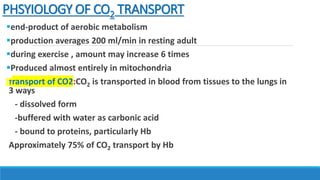
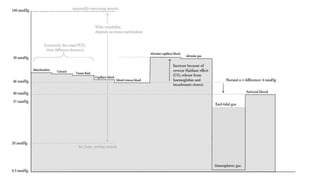
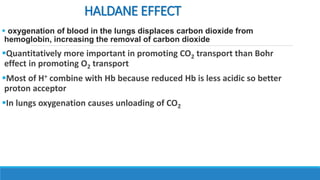
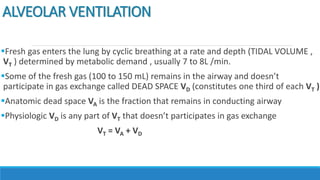
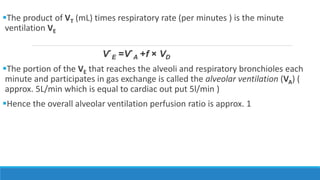
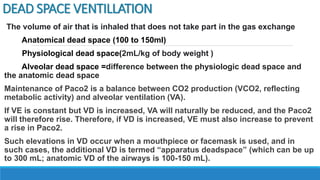
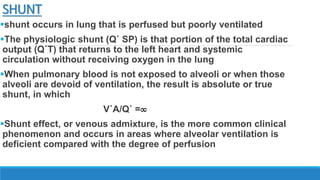
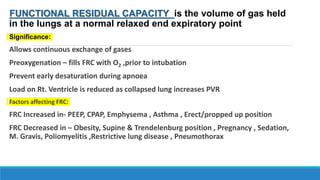
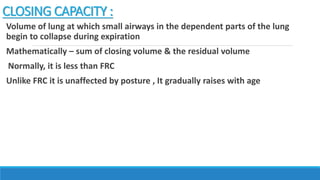
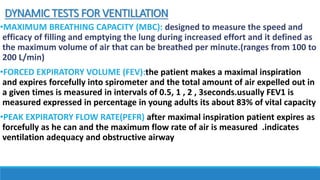
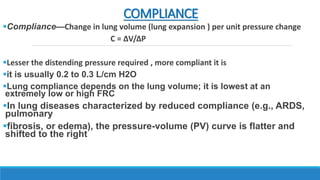
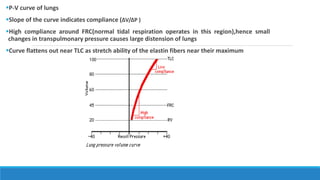
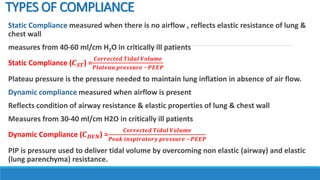
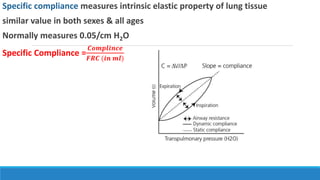
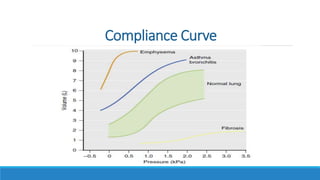
The document provides an extensive overview of respiratory physiology, focusing on the control of breathing by various centers in the brain, the role of chemoreceptors, and the mechanics of gas exchange in the lungs. It details the transport of oxygen and carbon dioxide in the blood, lung volumes and capacities, and the work of breathing, including the concepts of compliance and ventilation. Key principles such as the oxygen dissociation curve, the Bohr effect, and the physiological impact of shunts and dead space are also discussed.