This document provides information on various respiratory emergencies including their causes, signs and symptoms, and management strategies. Key points covered include:
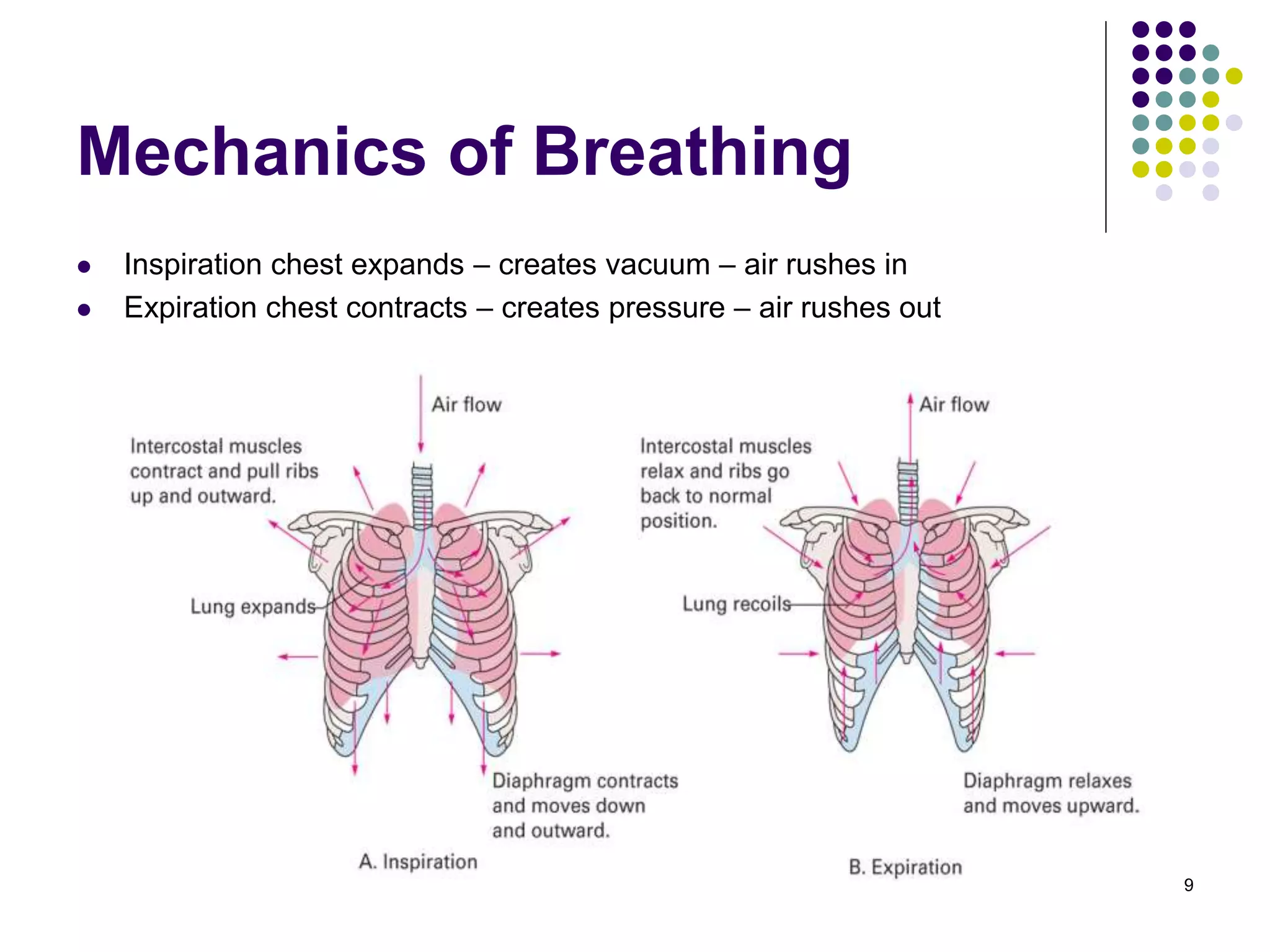
- The respiratory system functions to oxygenate the blood and remove carbon dioxide through ventilation, diffusion, and perfusion. Failure of any part of this process can cause respiratory emergencies.
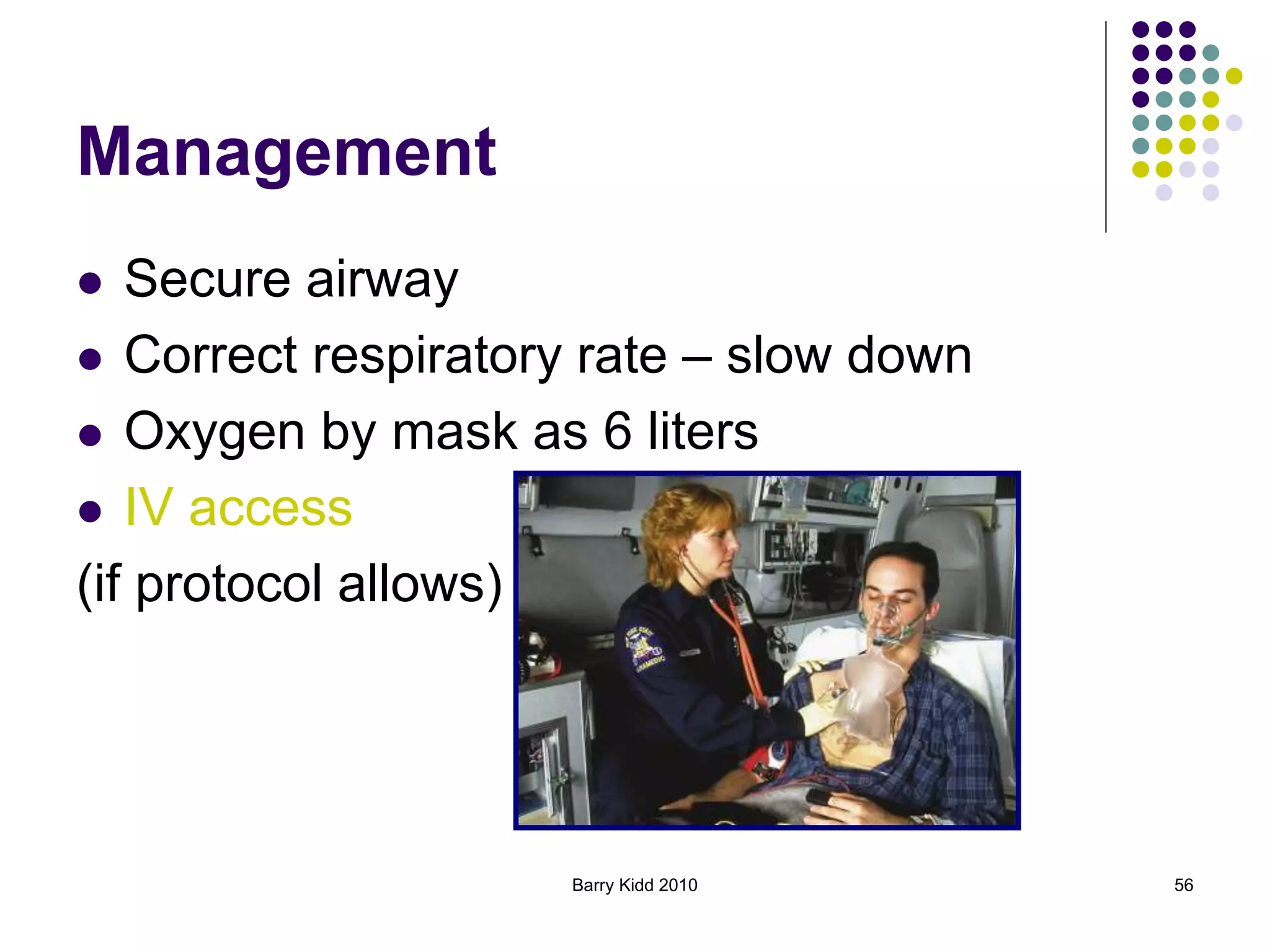
- Common respiratory emergencies discussed include upper airway obstruction, emphysema, asthma, pneumonia, toxic inhalation, and pulmonary embolism.
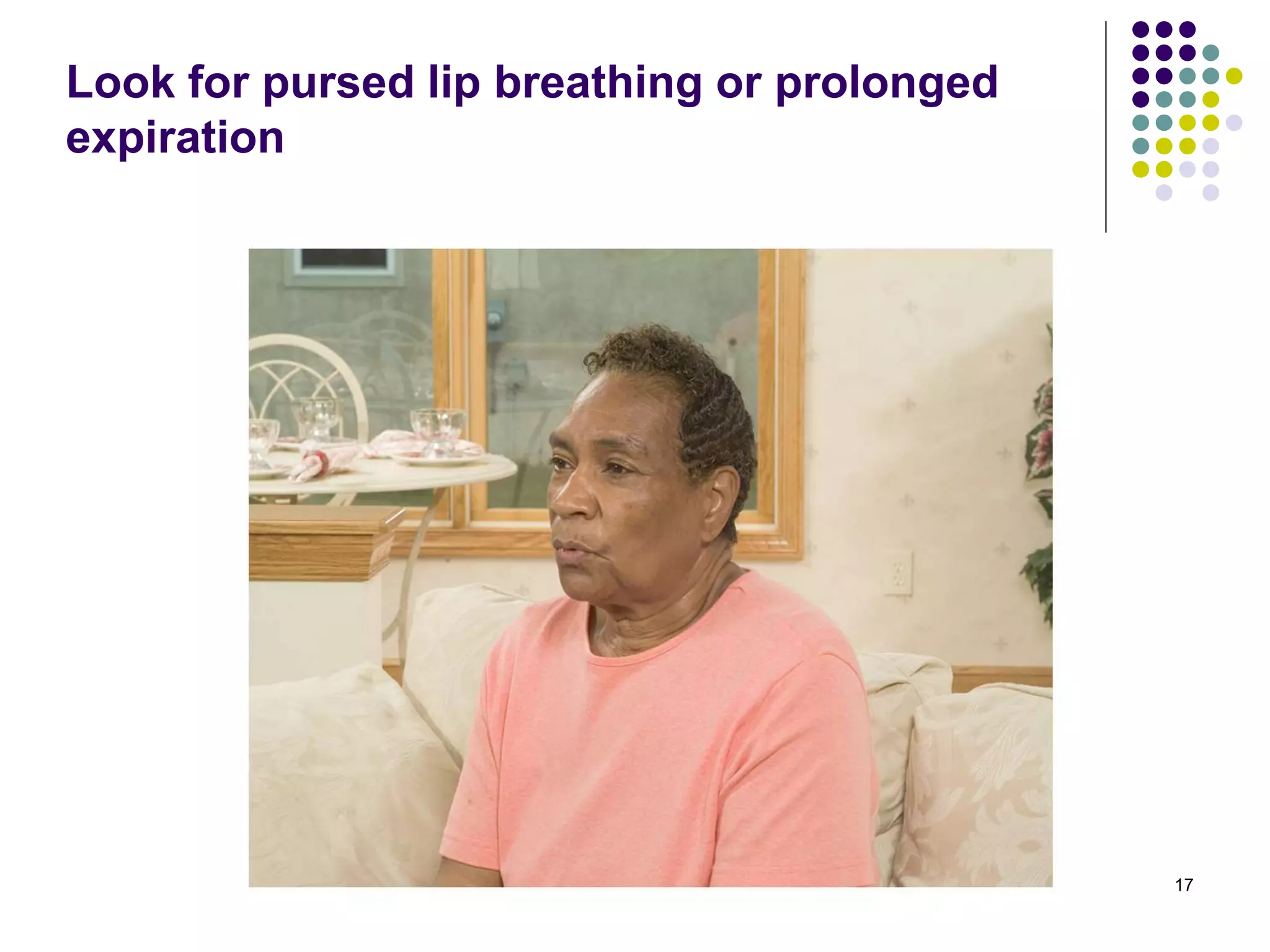
- Assessment involves evaluating the patient's airway, breathing, circulation, mental status and vital signs as well as taking a focused history. Signs and symptoms vary depending on the specific condition but may include dyspnea