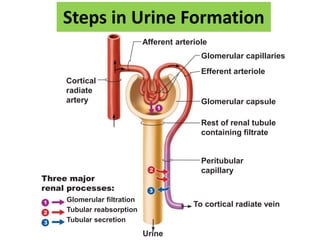
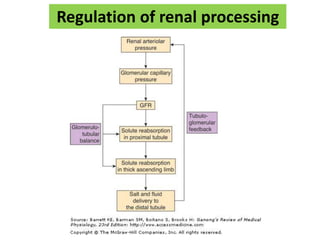
The document summarizes the key processes involved in urine formation:
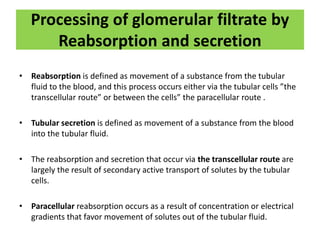
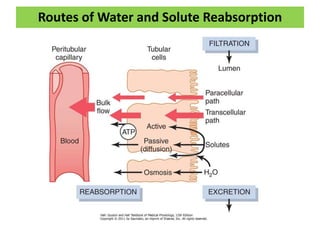
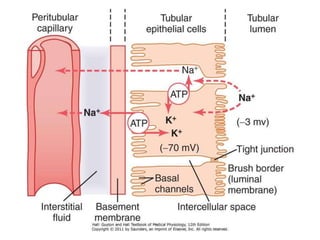
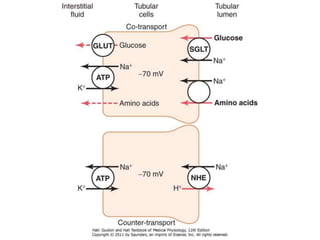
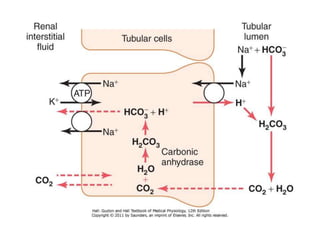
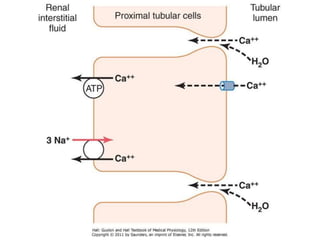
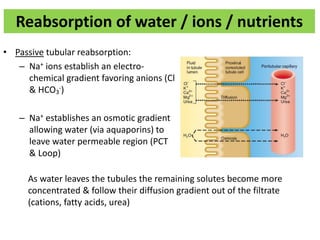
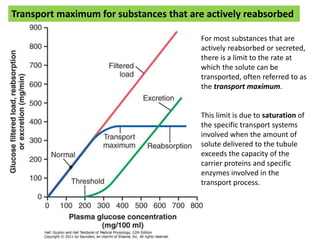
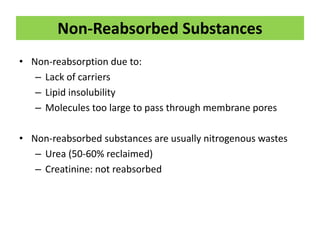
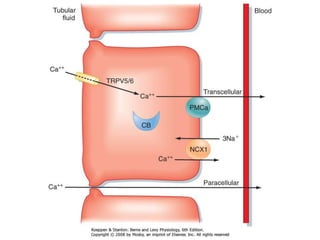
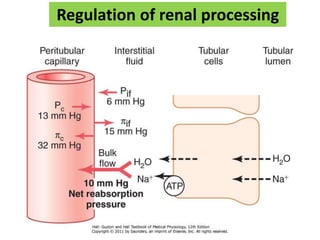
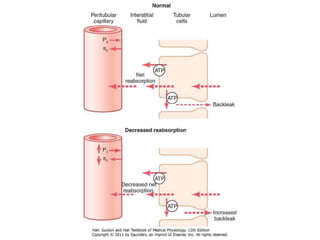
- Glomerular filtration, tubular reabsorption, and tubular secretion are the three major renal processes. Substances are reabsorbed or secreted across tubular cells via transcellular or paracellular routes.
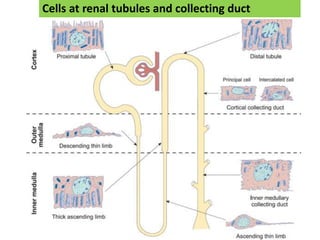
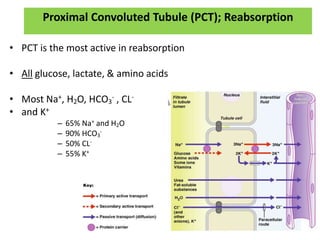
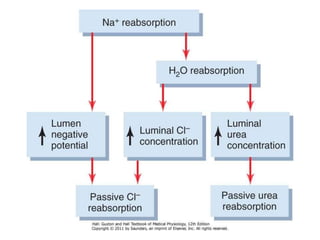
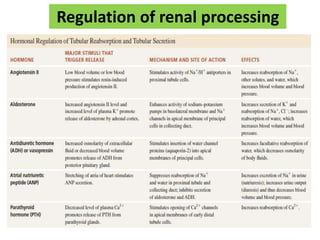
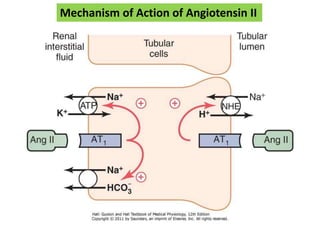
- The proximal convoluted tubule reabsorbs the majority of filtered sodium, water, bicarbonate, chloride and potassium.
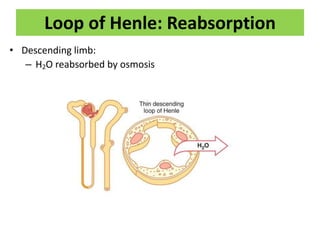
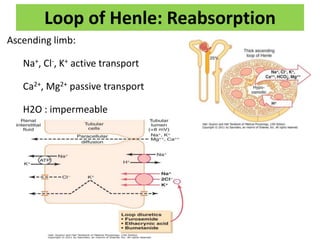
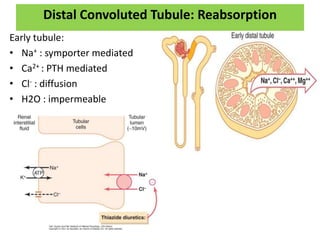
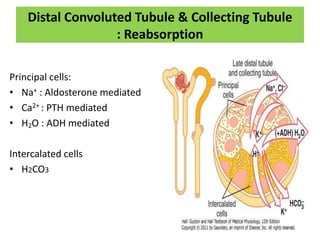
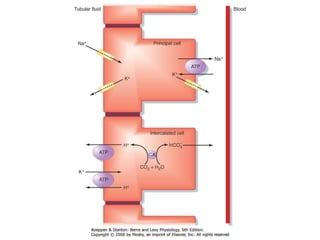
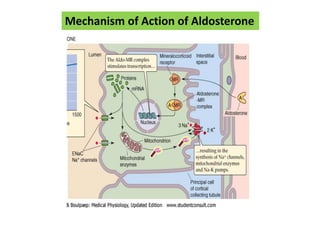
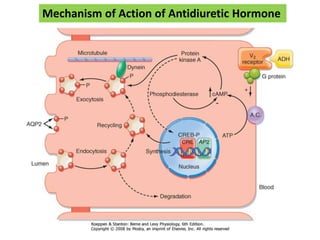
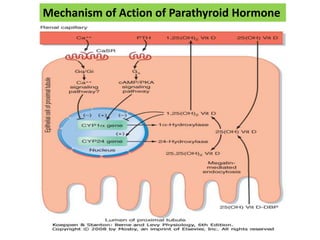
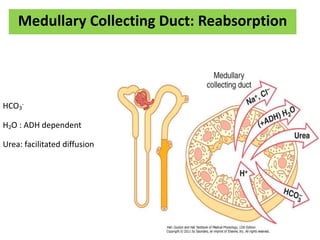
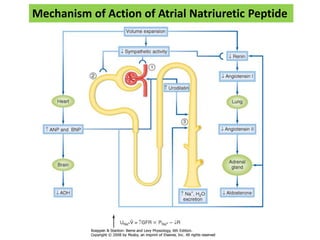
- The loop of Henle and distal convoluted tubule further regulate reabsorption and secretion of ions and water, facilitated by hormones like aldosterone and antidiuretic hormone.
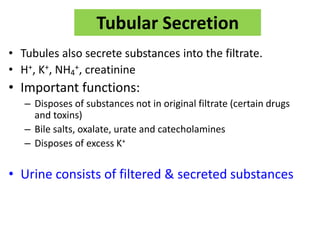
- Tubular secretion disposes of substances not in the original filtrate like drugs,