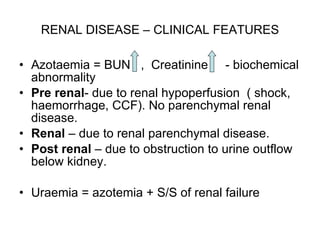
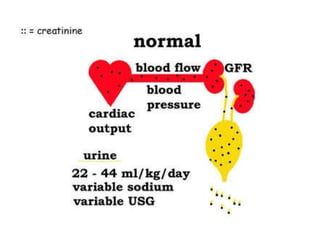
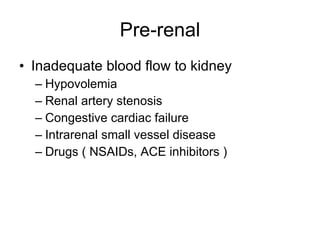
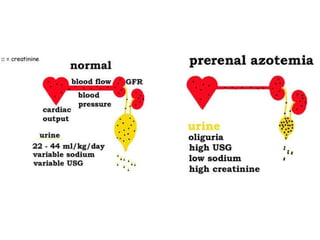
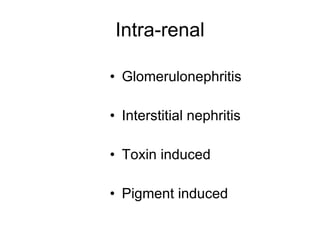
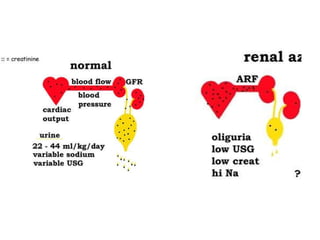
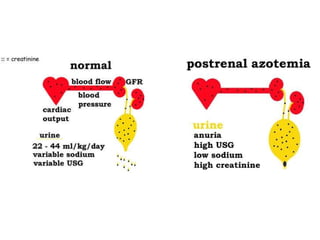
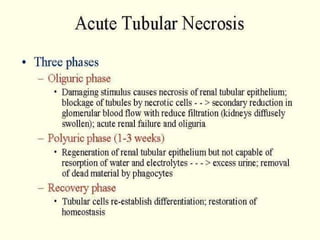
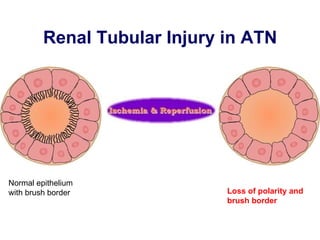
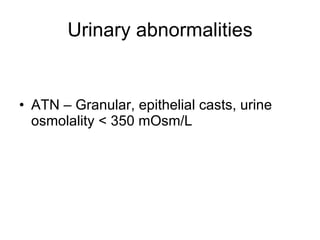
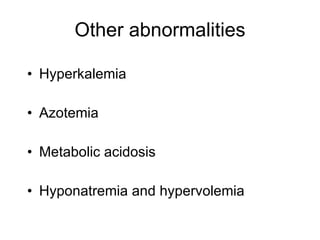
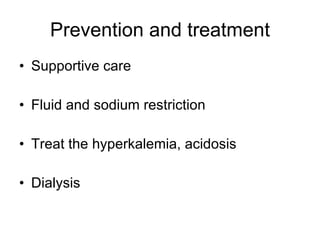
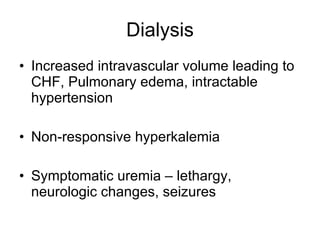
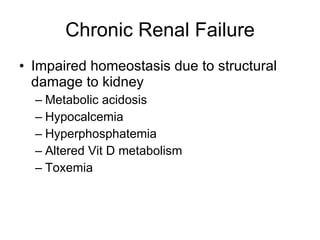
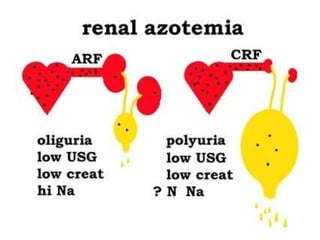
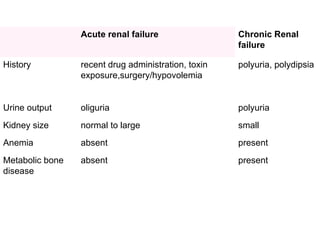
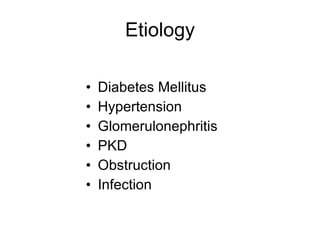
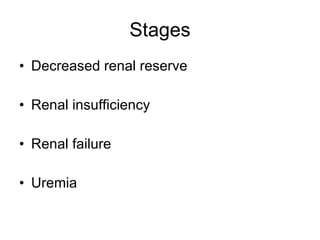
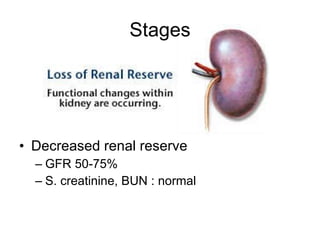
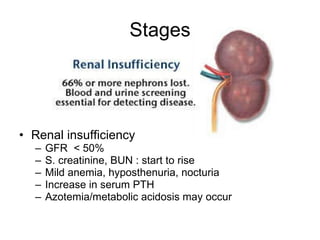
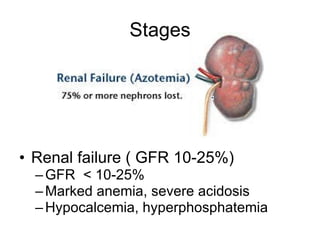
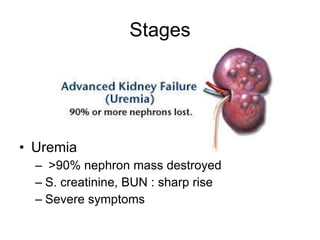
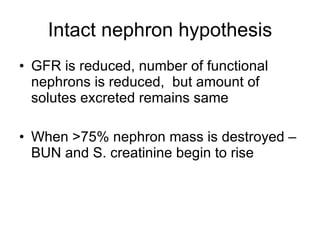
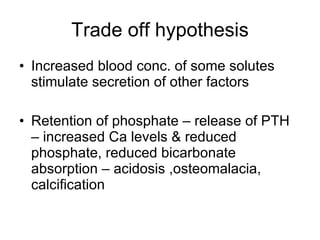
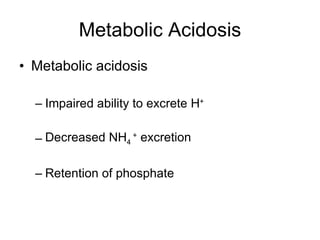
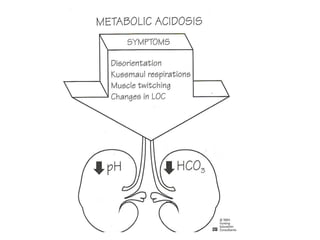
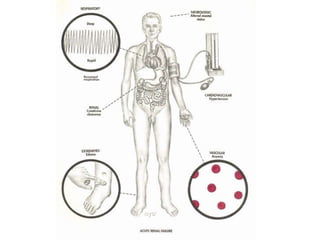
There are two main types of renal failure - acute and chronic. Acute renal failure is a sudden onset condition characterized by oliguria/anuria and a rapid rise in BUN and creatinine levels. Chronic renal failure is a long-term condition that impairs homeostasis due to structural kidney damage and leads to metabolic complications like acidosis, hypocalcemia, and hyperphosphatemia. The causes and stages of both acute and chronic renal failure are described.