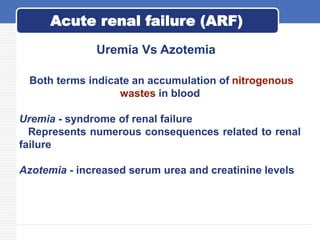
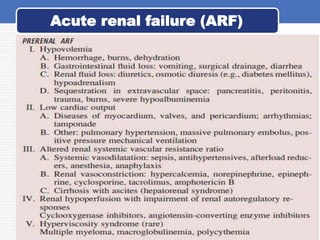
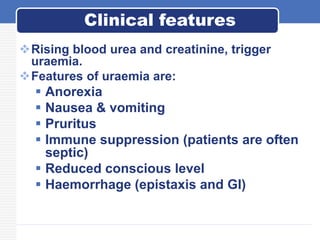
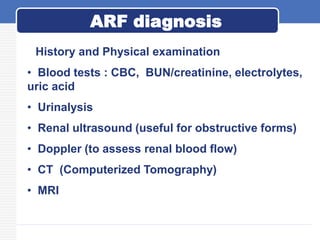
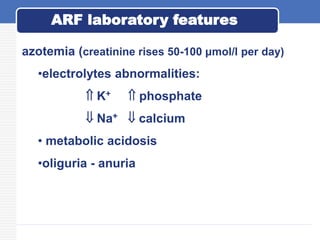
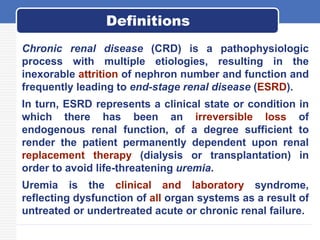
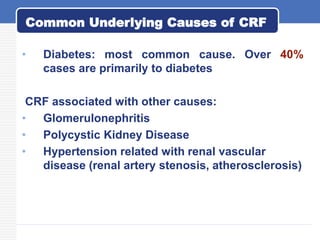
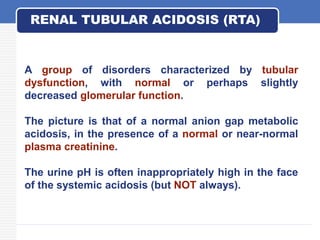
This document provides an overview of common renal disorders, including acute renal failure (ARF), chronic renal failure, nephrotic syndrome, nephrolithiasis, and renal tubular acidosis. ARF is characterized by a rapid decline in glomerular filtration rate and is divided into prerenal, intrinsic renal, and postrenal types. Chronic renal failure is usually caused by diabetes or glomerulonephritis and results in metabolic abnormalities and uremic syndrome. Nephrotic syndrome involves proteinuria, hypoalbuminemia, edema, and hyperlipidemia due to increased glomerular permeability. Nephrolithiasis is caused by supersaturation of urine leading to stone formation,