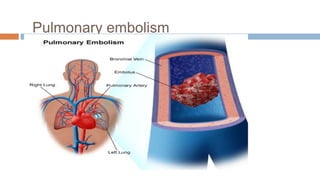
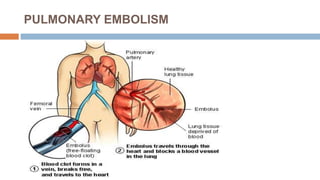
Pulmonary embolism occurs when a blood clot forms in the veins (usually in the legs) and travels to the lungs, blocking blood flow. Risk factors include prolonged immobility, recent surgery or trauma, older age, and certain medical conditions. Symptoms can range from mild chest pain to life-threatening issues like respiratory failure. Diagnosis involves tests like chest x-rays, CT scans, and blood tests. Treatment may include blood thinners, clot-busting drugs, or occasionally surgery to remove large clots. Nursing care focuses on preventing further clots, reducing pain and anxiety, and monitoring for complications of treatment.