This document provides tips and instructions for using a PowerPoint presentation (PPT) on pulmonary embolism:
1. The PPT can be freely downloaded, edited, and modified. It includes some blank slides for notes.
2. The instructor should first show blank slides to elicit what students already know, then show slides with content.
3. This approach, repeating with questions and answers, allows for an active learning session.
4. The PPT can also be used for self-study, with notes and bibliography provided.




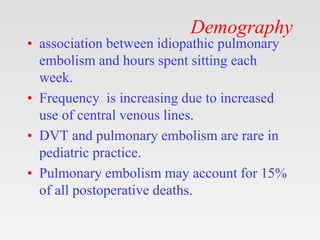

![Atypical Symptoms
• Seizures
• Syncope
• Abdominal pain
• Fever
• Productive cough
• Wheezing
• Decreasing level of
consciousness
• New onset of atrial
fibrillation
• Hemoptysis
• Flank pain [1]
• Delirium (in elderly
patients) [2]](https://image.slidesharecdn.com/pulmonaryembolism-221115061433-a0c7669e/85/Pulmonary-Embolism-pptx-18-320.jpg)
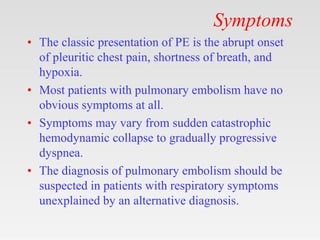
![Physical signs
• Tachypnea
(respiratory rate
>16/min): 96%
• Rales: 58%
• Accentuated second
heart sound: 53%
• Tachycardia (heart
rate >100/min): 44%
• Fever (temperature
>37.8°C [100.04°F]):
43%
• Diaphoresis: 36%
• S3 or S4 gallop: 34%
• Clinical signs and
symptoms suggesting
thrombophlebitis: 32%
• Lower extremity
edema: 24%
• Cardiac murmur: 23%
• Cyanosis: 19](https://image.slidesharecdn.com/pulmonaryembolism-221115061433-a0c7669e/85/Pulmonary-Embolism-pptx-19-320.jpg)