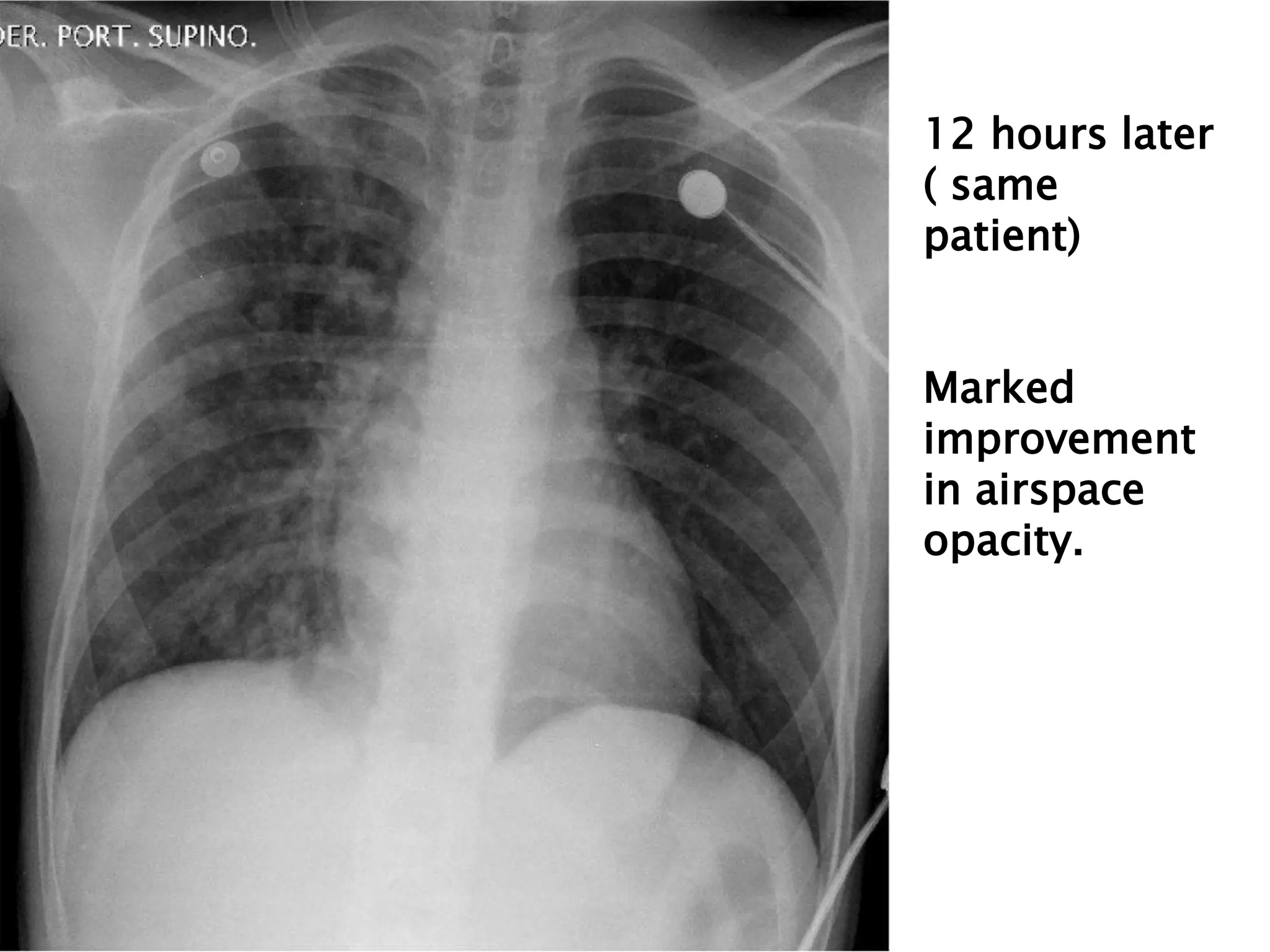
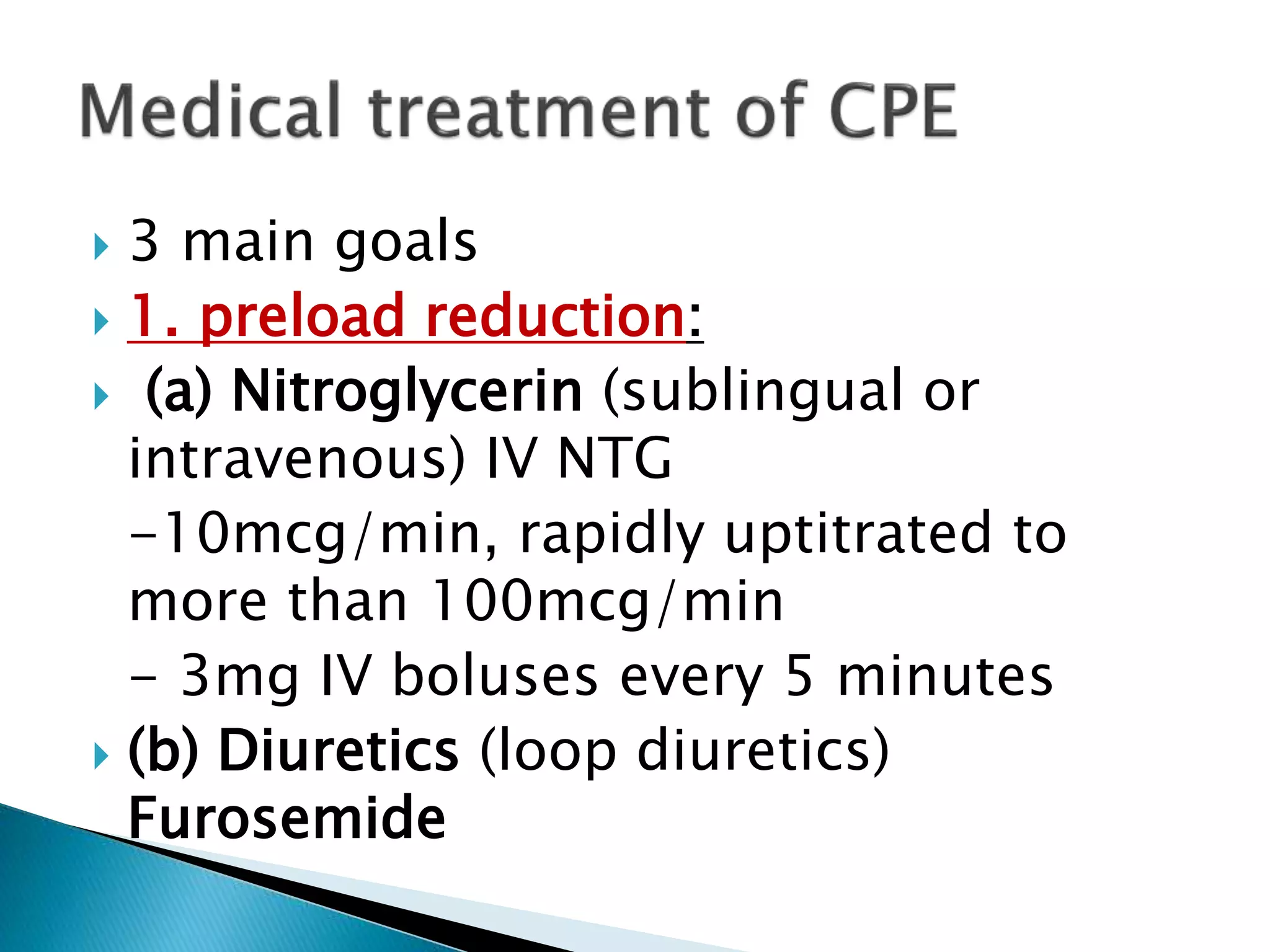
Pulmonary edema is fluid accumulation in the lungs caused by fluid leaking from blood vessels into the lungs. It can be cardiogenic (caused by heart problems increasing blood pressure in the lungs) or non-cardiogenic. Symptoms include shortness of breath, cough, and cyanosis. Diagnosis involves chest x-ray, echocardiogram, and measuring wedge pressure. Treatment focuses on reducing preload on the heart, lowering afterload, and providing supportive care like oxygen. Outcomes depend on the underlying cause but most cardiogenic cases resolve within 3 days with medical management.