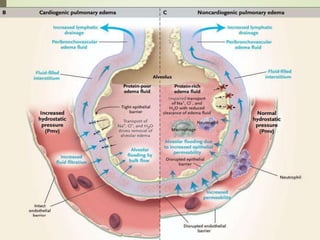
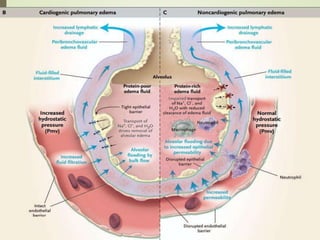
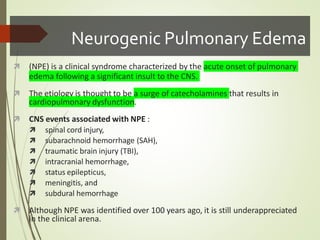
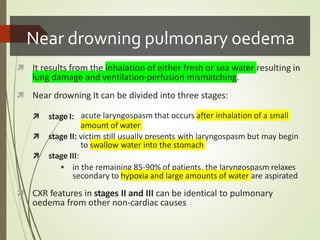
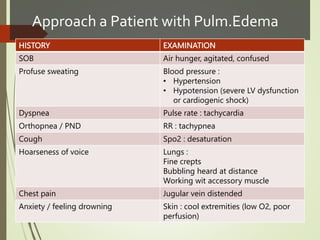
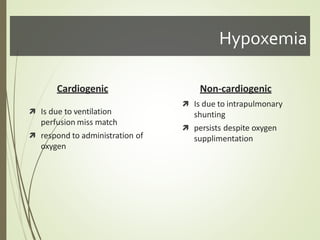
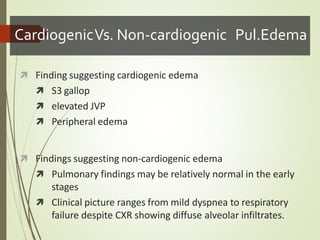
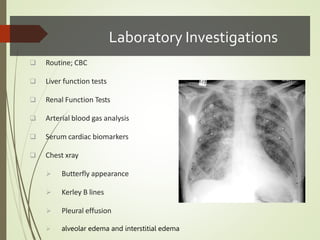
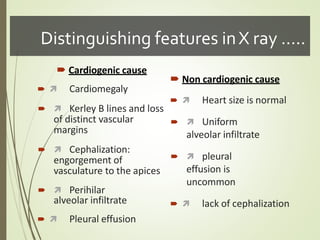
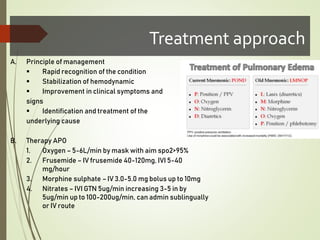
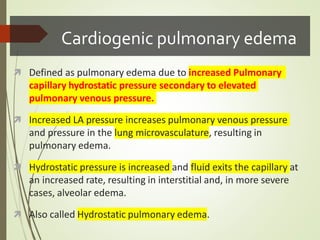
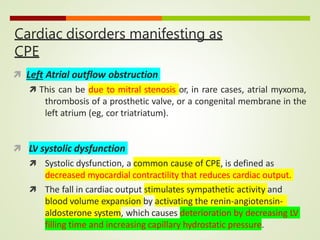
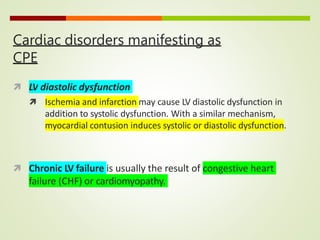
Acute pulmonary edema can be either cardiogenic or non-cardiogenic in origin. Cardiogenic pulmonary edema is caused by elevated pulmonary capillary hydrostatic pressure due to conditions that increase left atrial pressure like heart failure, myocardial infarction, or valvular disease. It presents with dyspnea, crackles on exam, and chest x-ray findings of vascular congestion and fluid in the lungs. Treatment involves oxygen, diuretics, vasodilators, and inotropes. Non-cardiogenic pulmonary edema is caused by damage to the lung capillaries from conditions like near-drowning or neurogenic injury and presents with hypoxemia that does not resolve with oxygen alone.

![ Causes of acute exacerbations of CPE
Acute myocardial infarction (MI) or ischemia
Patient noncompliance with dietary restrictions (eg, dietary salt
restrictions)
Patient noncompliance with medications (eg, diuretics)
Severe anemia with underlying cardiac ilness
Sepsis
Thyrotoxicosis
Myocarditis
Myocardial toxins (eg, alcohol, cocaine, chemotherapeutic agents
such as doxorubicin [Adriamycin], trastuzumab [Herceptin])
Chronic valvular disease, aortic stenosis, aortic regurgitation, and
mitral regurgitation](https://image.slidesharecdn.com/pulmonaryedemagokull-230222235525-d29c42fb/85/pulmonary-edema-gokull-pptx-9-320.jpg)