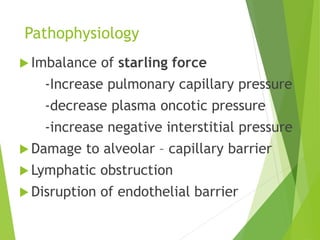
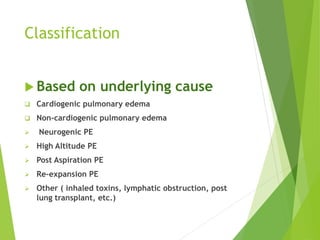
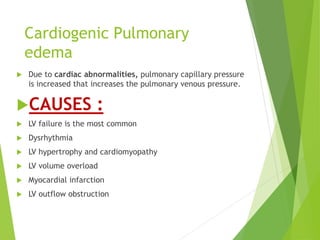
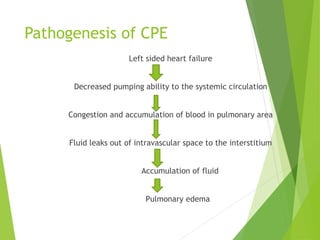
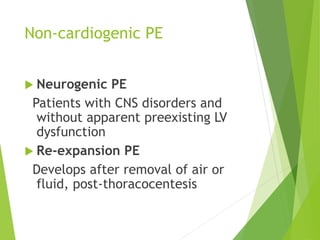
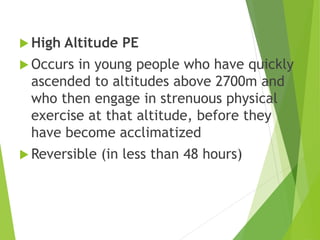
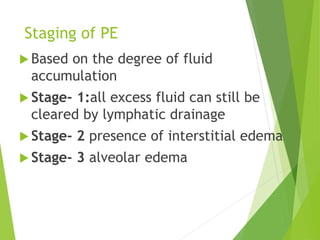
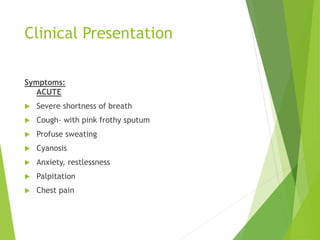
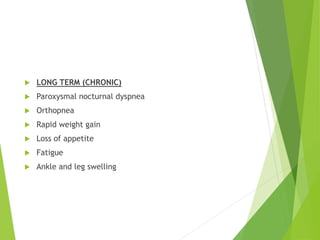
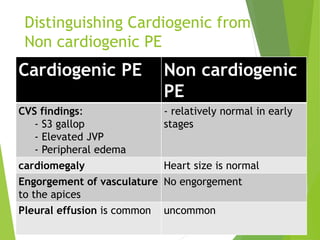
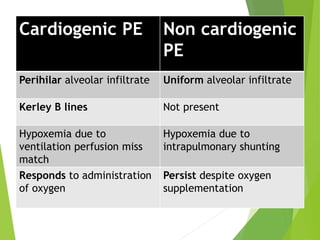
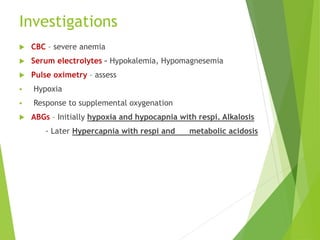
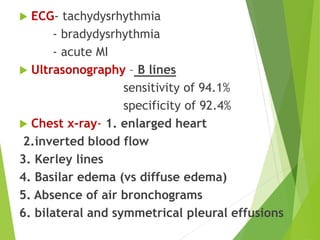
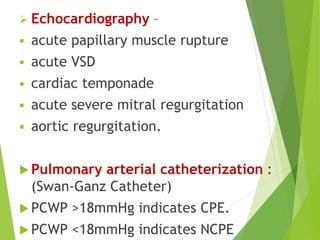
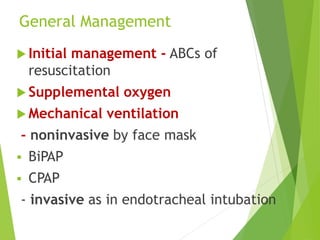
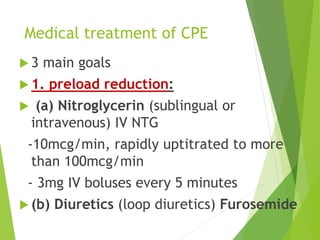
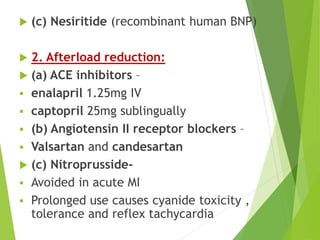
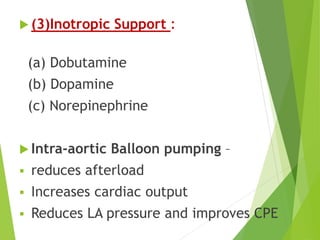
Pulmonary edema is a condition marked by fluid accumulation in the lungs, resulting from various causes, including cardiogenic and non-cardiogenic factors. Symptoms include severe shortness of breath, cough with pink frothy sputum, and cyanosis, with complications such as leg edema and respiratory arrest. Management strategies focus on oxygen supplementation, mechanical ventilation, and medications to reduce preload and afterload.