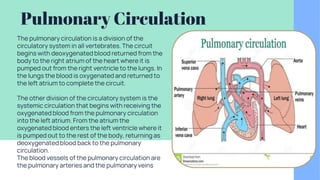
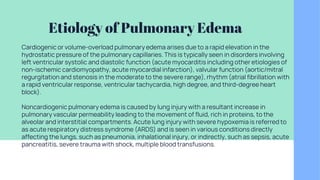
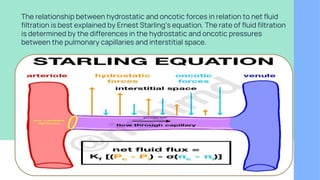
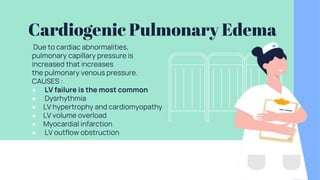
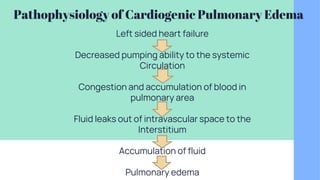
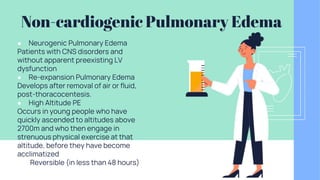
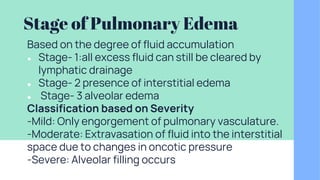
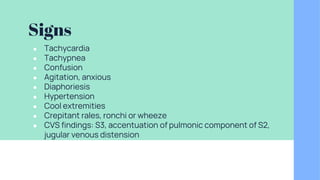
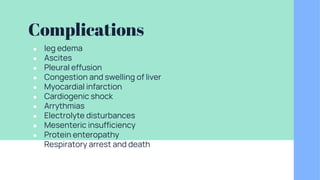
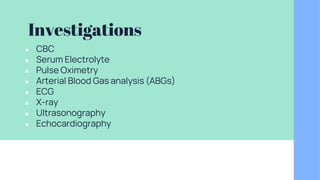
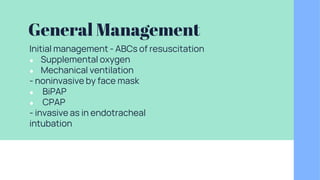
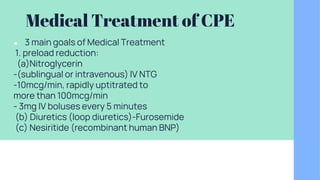
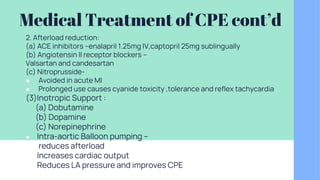
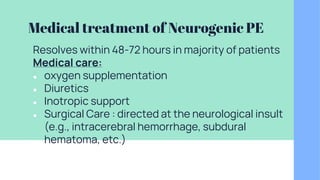
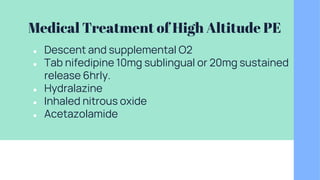
The document discusses pulmonary circulation, pleural fluid, and pulmonary edema. It defines these topics and describes their pathophysiology. Pulmonary circulation carries deoxygenated blood from the heart to the lungs to be oxygenated. Pleural fluid lubricates the lungs during breathing, and too much fluid can cause difficulty breathing. Pulmonary edema is fluid accumulation in the lungs, with cardiogenic edema due to heart issues impairing fluid removal and non-cardiogenic due to lung injury. Signs, treatments, and complications are also outlined.