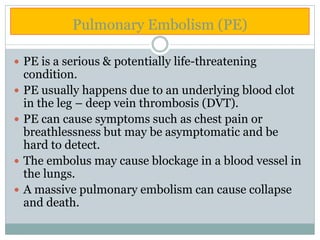
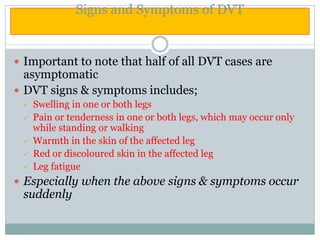
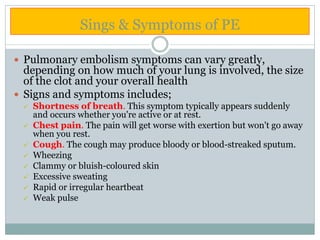
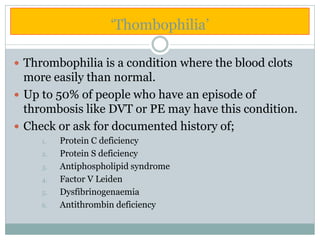
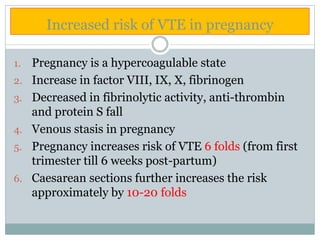
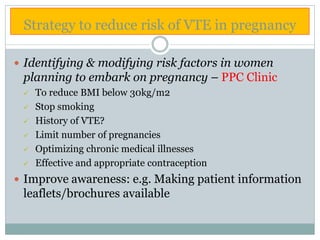
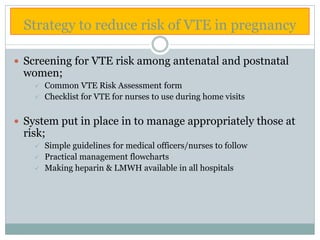
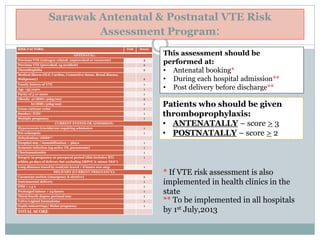
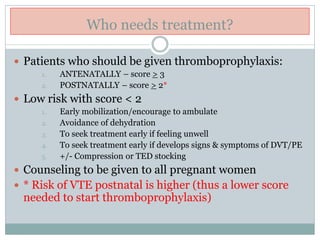
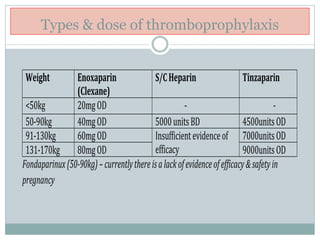
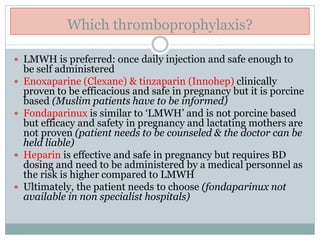
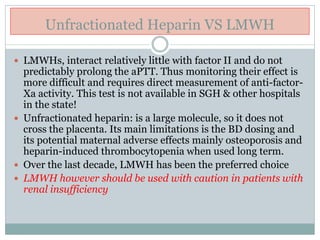
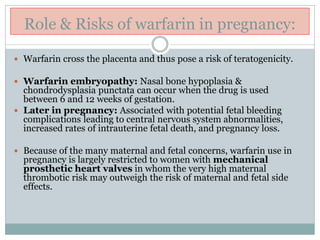
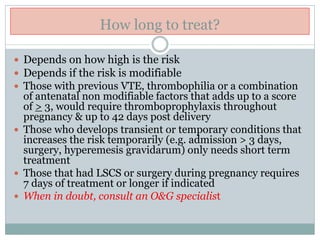
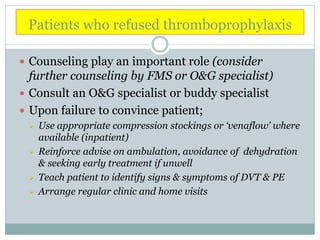
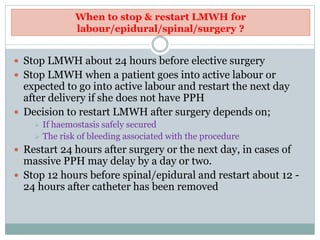
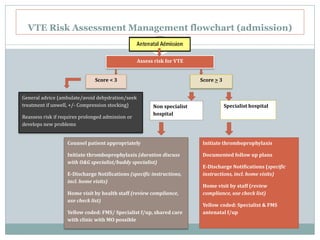
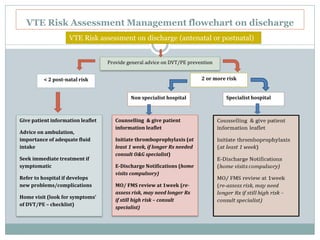
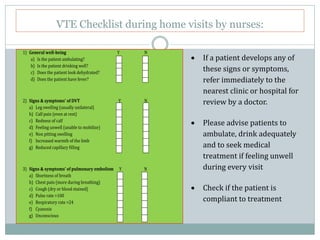
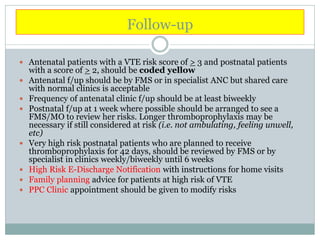
The document outlines the rising incidence of pulmonary embolism (PE) as a critical cause of maternal mortality, particularly in Malaysia and Sarawak, where specific risk factors and prevention strategies are emphasized. It details guidelines for assessing and managing venous thromboembolism (VTE) risk during the antenatal and postnatal periods, including thromboprophylaxis recommendations based on patient risk scores. A comprehensive protocol for risk assessment, monitoring, and patient education is proposed to mitigate the significant but preventable risk of VTE-related maternal deaths.