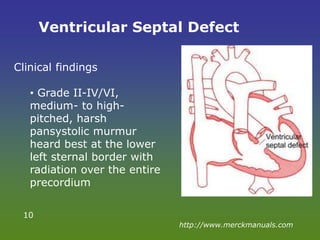
This document discusses congenital heart disease (CHD), which affects nearly 1% of births annually in the United States. It outlines the epidemiology, anatomy, types, clinical approach, history taking, physical exams, investigations and general management of CHD. The most common type is ventricular septal defect. While about 95% of babies with non-critical CHD are expected to survive to 18 years, only 69% of those with critical CHD are expected to survive. The document describes several specific types of CHDs in detail, including their typical features, exams, treatments and management approaches.


![EPIDEMIOLOGY
• CHDs affect nearly 1% of or about 40,000 births
per year in the United States
• The most common type of heart defect is a
ventricular septal defect (VSD)
• About 95% of babies born with a non-critical CHD
are expected to survive to 18 years of age [2012]
• About 69% of babies born with critical CHDs are
expected to survive to 18 years of age [2012]
http://www.cdc.gov
• A study on under five deaths in Malaysia in the
year 2006 showed that 10% of mortality was
directly related to CHD - http://mjpch.com
3](https://image.slidesharecdn.com/congenitalheartdisease-141220205557-conversion-gate01/85/Congenital-heart-disease-3-320.jpg)