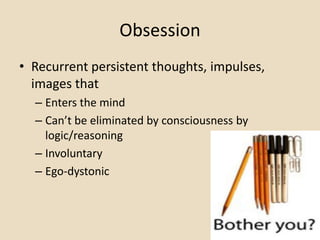
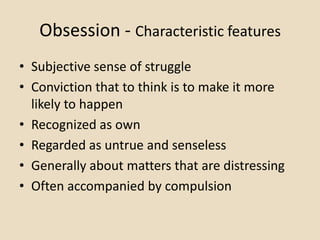
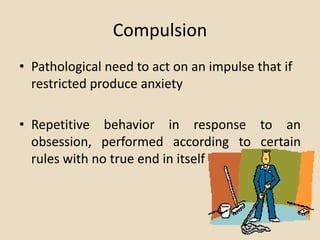
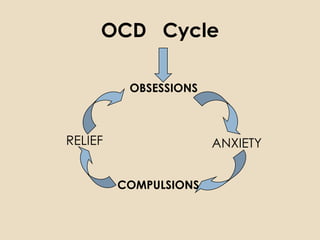
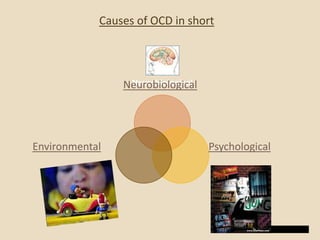
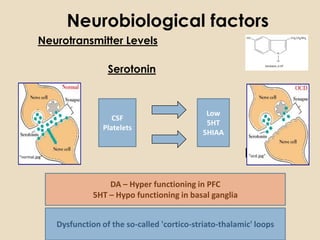
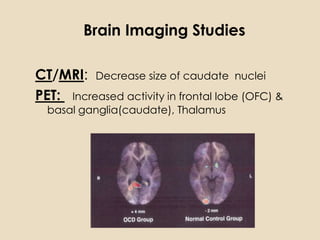
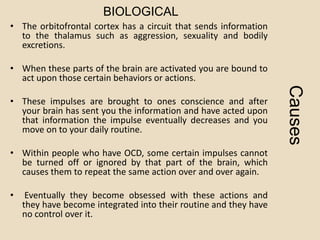
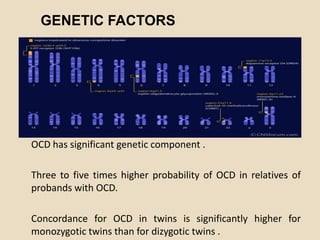
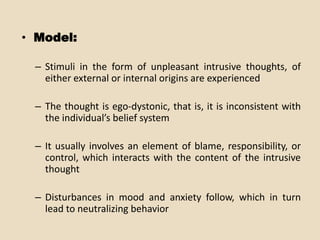
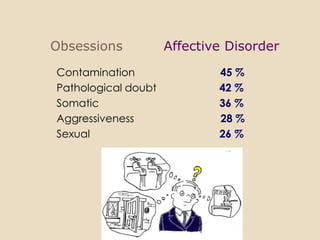
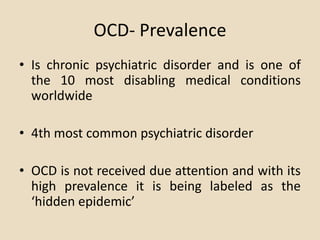
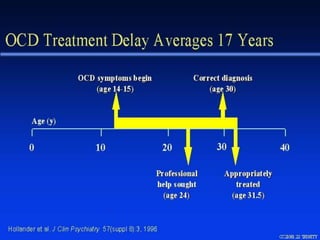
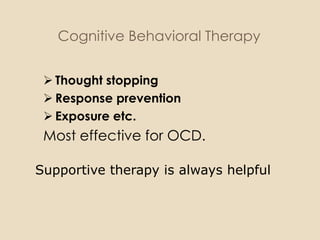
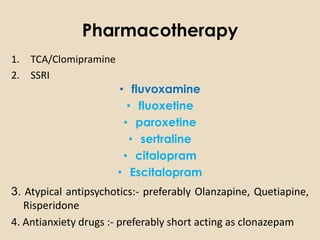
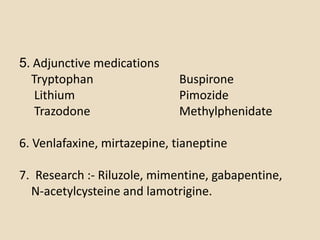
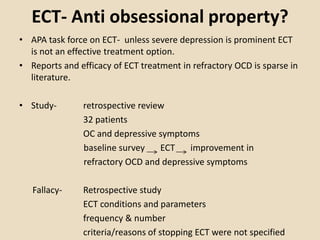
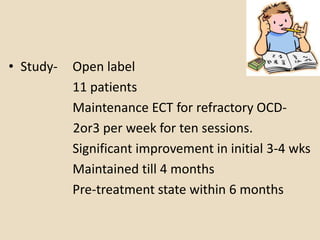
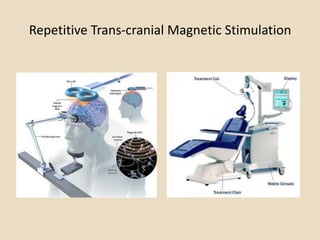
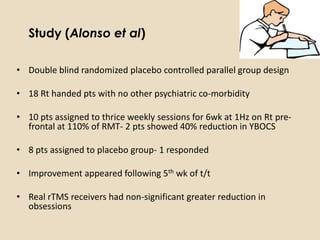
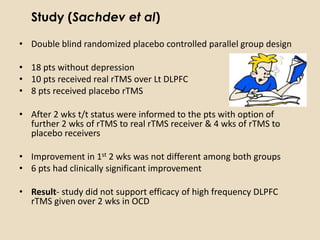
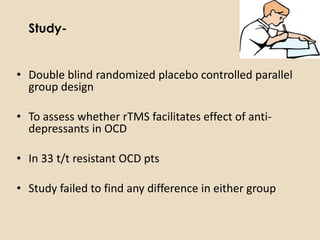
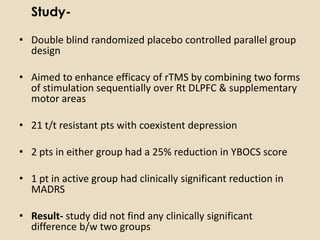
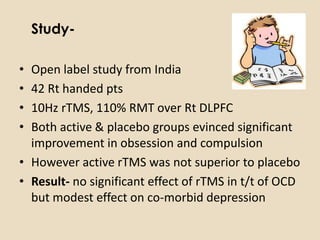
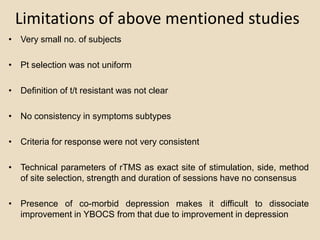
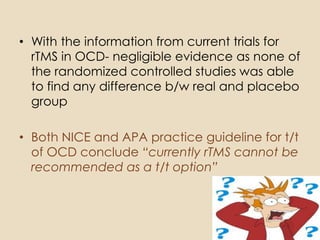
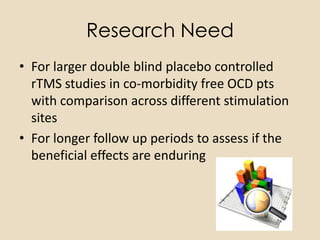
Obsessive Compulsive Disorder (OCD) is an anxiety disorder characterized by recurrent, unwanted thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) performed in response to these thoughts. The obsessions or compulsions significantly interfere with daily life. OCD has been linked to imbalances in neurotransmitters like serotonin and dopamine in the brain, as well as genetic and environmental factors. Treatment involves psychotherapy like cognitive behavioral therapy and medication like selective serotonin reuptake inhibitors. Other potential treatments under research include repetitive transcranial magnetic stimulation and electroconvulsive therapy, but more studies are still needed to establish their efficacy for OCD.