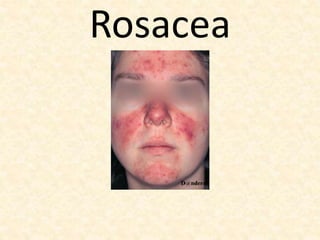
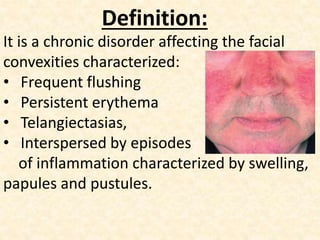
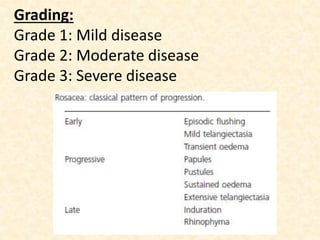
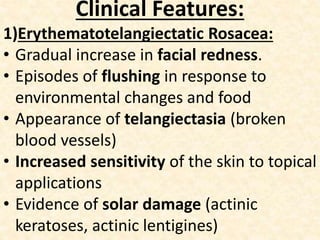
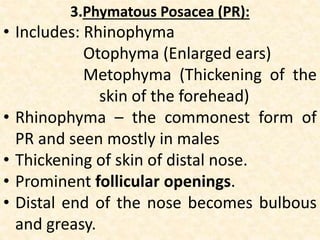
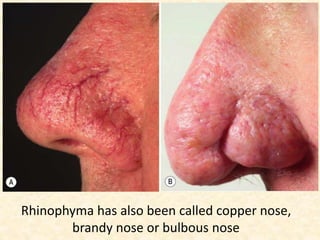
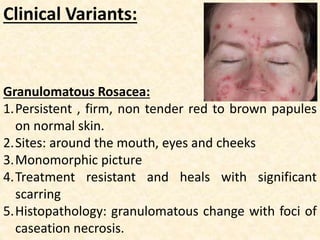
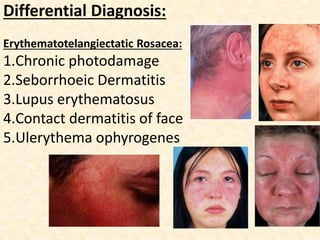
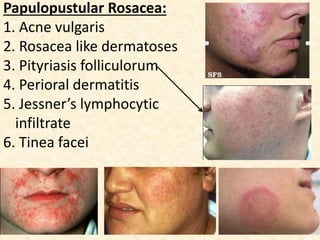
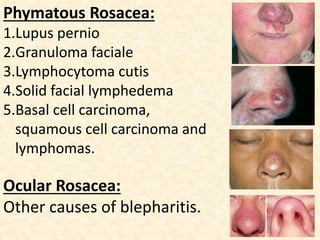
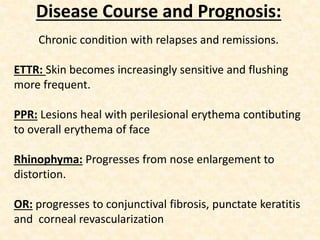
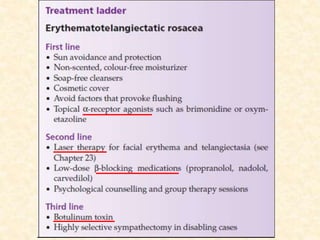
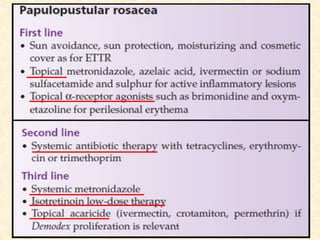
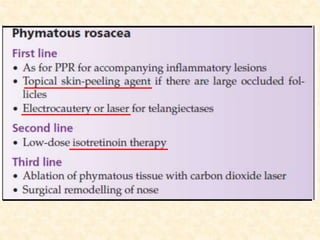
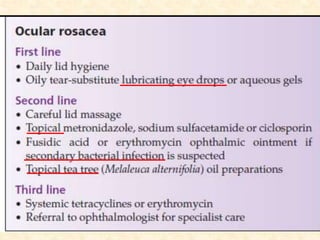
Rosacea is a chronic skin condition that affects the face, characterized by flushing, persistent redness, small visible blood vessels, pimples or bumps, and thickened skin, especially on the nose, cheeks, chin, and forehead. It is classified into subtypes based on symptoms such as erythema, papules and pustules, and phymatous changes. Treatment aims to reduce inflammation and prevent worsening of symptoms. Left untreated, rosacea can progress and cause permanent changes to the facial structure over many years.