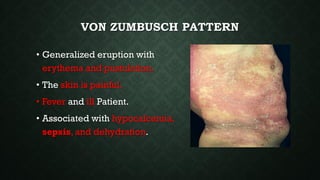
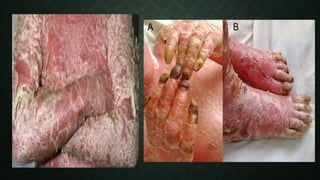
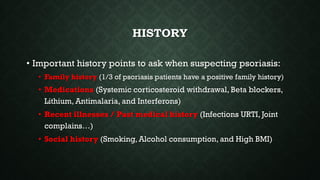
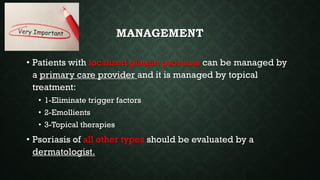
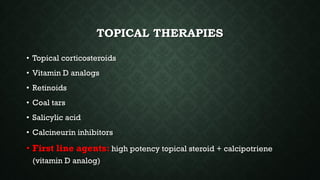
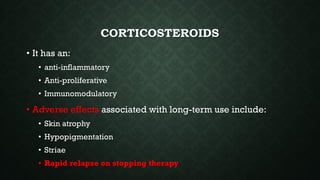
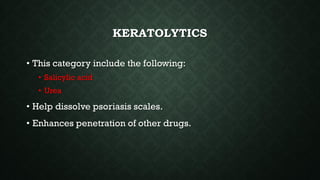
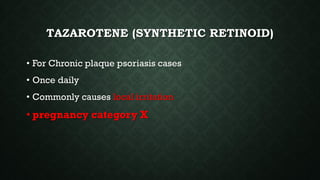
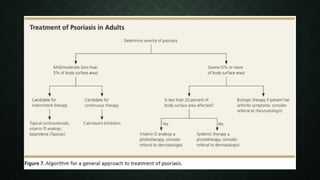
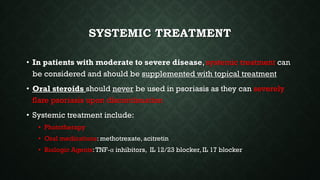
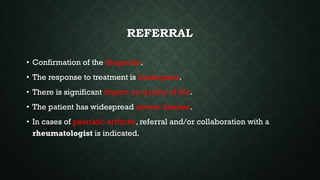
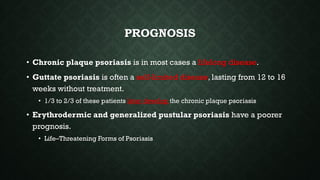
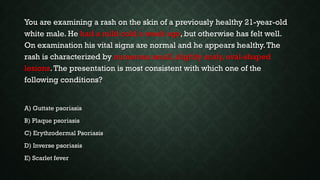
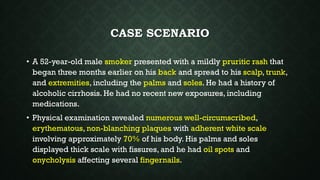
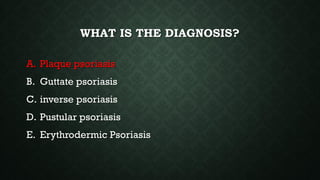
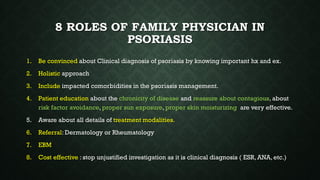
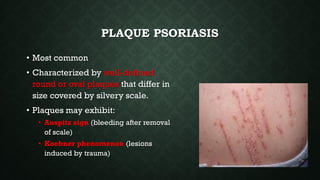
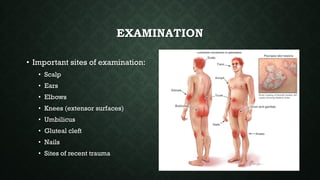
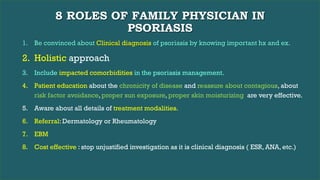
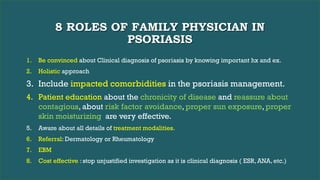
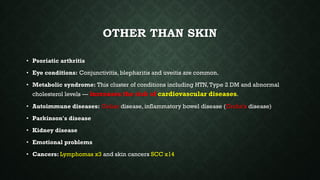
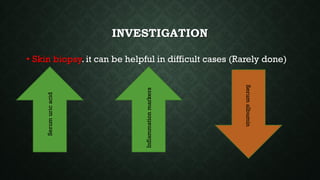
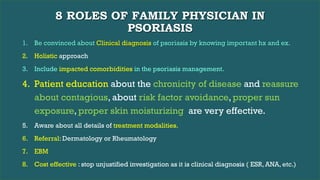
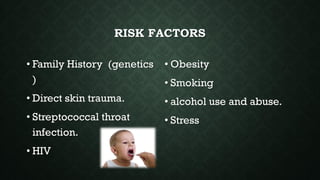
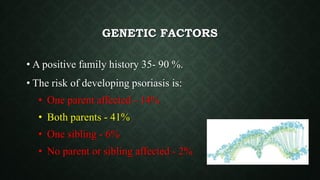
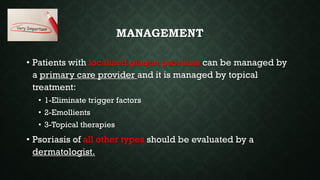
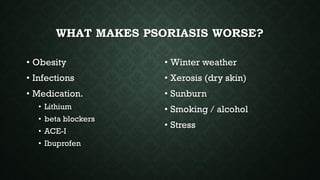
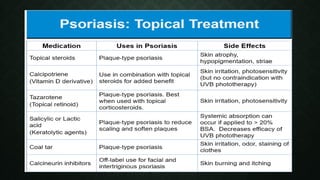
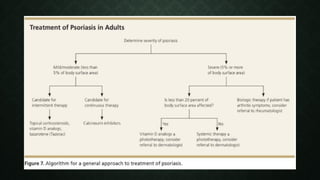
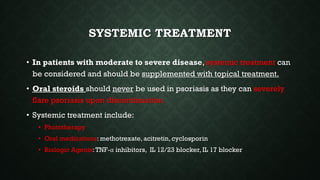
The patient, a 52-year-old male smoker with a history of alcoholic cirrhosis, presented with a widespread pruritic rash involving 70% of his body consistent with erythrodermic psoriasis. As the family physician's roles include making an accurate clinical diagnosis of psoriasis, taking a holistic approach to management, educating patients, and knowing treatment options including when referral is needed, the physician must determine the appropriate management for this severe case of erythrodermic psoriasis.