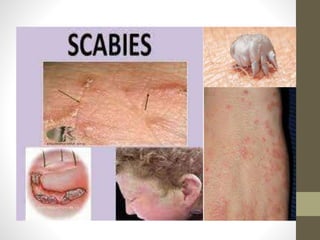
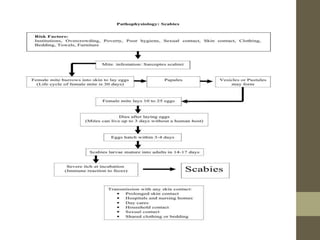
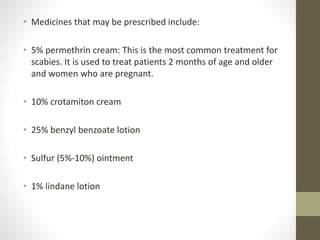
Eczema, or dermatitis, is a non-contagious skin condition affecting 10-20% of infants and 3% of adults, characterized by itchy, inflamed skin and various types such as atopic dermatitis and contact dermatitis. Scabies, caused by the sarcoptes scabiei mite, is highly contagious and causes severe itching, with common treatments including topical medications and careful cleaning of clothing and bedding to prevent re-infestation. Both conditions require management of symptoms, with eczema often treated through moisturizers and antihistamines, while scabies necessitates specific topical treatments prescribed by a dermatologist.