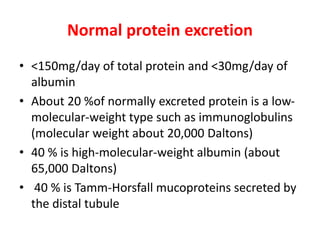
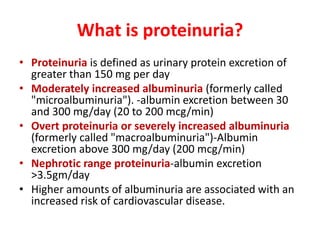
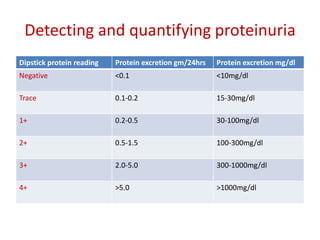
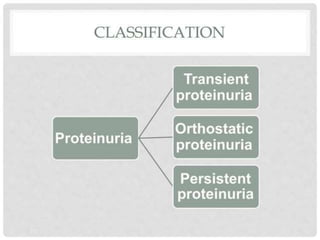
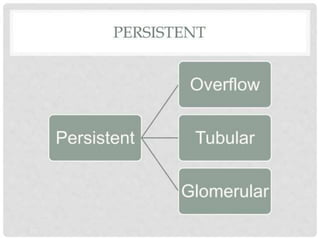
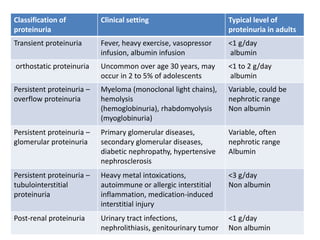
The document discusses proteinuria, or excess protein in the urine. It defines normal protein excretion and levels of proteinuria like microalbuminuria and nephrotic range proteinuria. There are three main mechanisms of proteinuria - glomerular, tubular, or overflow. Glomerular issues allow albumin and immunoglobulins into the urine while tubular diseases prevent reabsorption of low molecular weight proteins. The document also covers evaluating proteinuria using urine dipsticks, microscopic analysis of urine sediments, and considering causes of proteinuria.