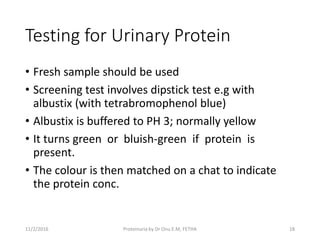
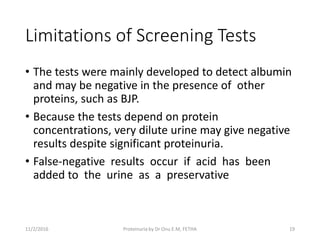
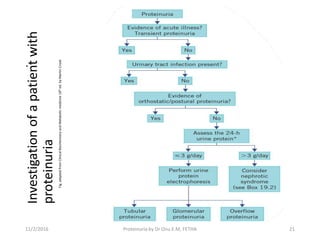
The document provides an in-depth clinical presentation on proteinuria, defining it as excessive protein in urine, with normal levels being less than 150 mg/24 hours. It discusses types of proteinuria, testing methods, limitations of screening tests, and treatment options, emphasizing the importance of identifying underlying causes and potential referrals to a nephrologist. Key classifications include glomerular and tubular proteinuria, with respective diagnostic features and management strategies outlined.