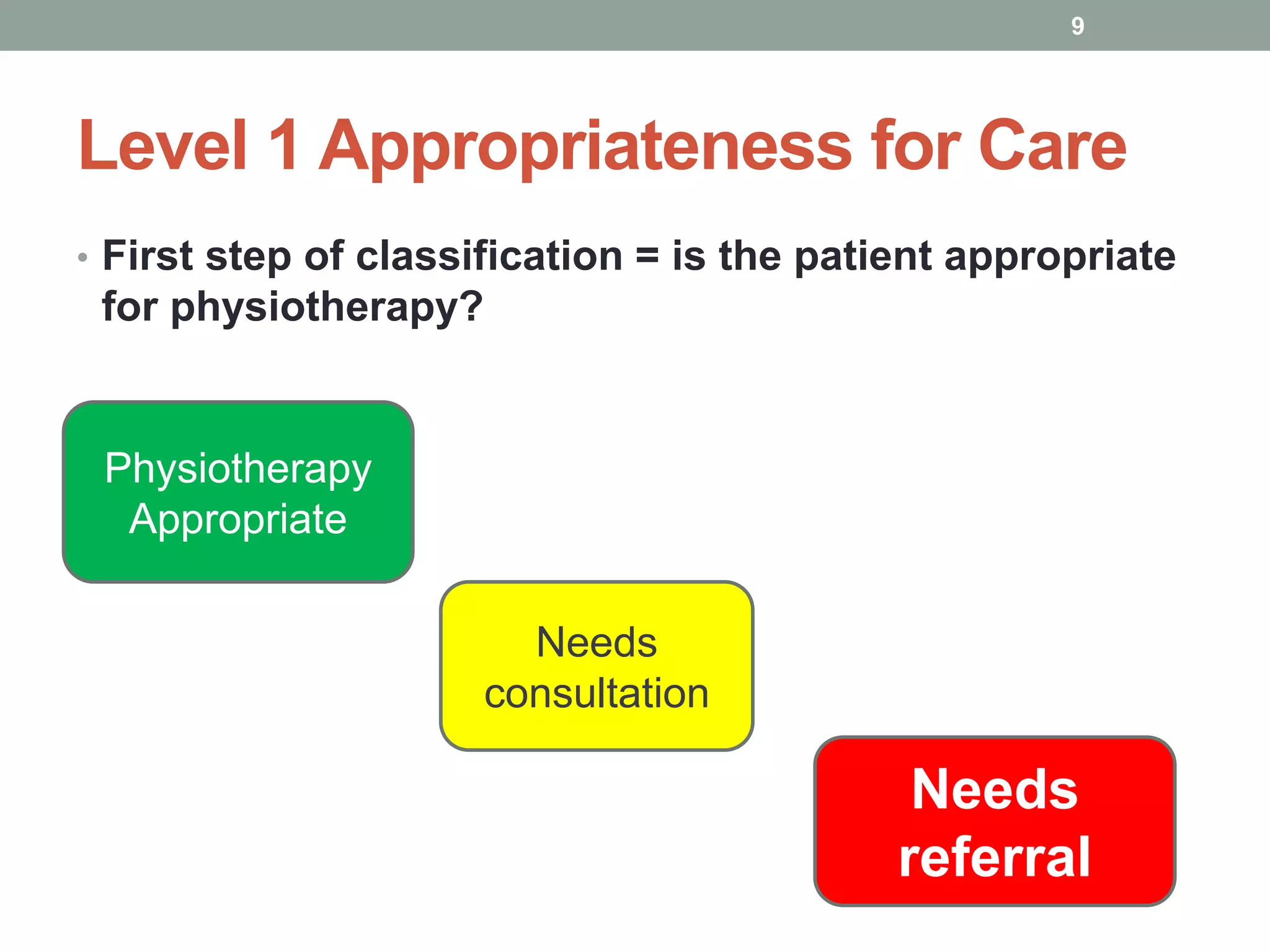
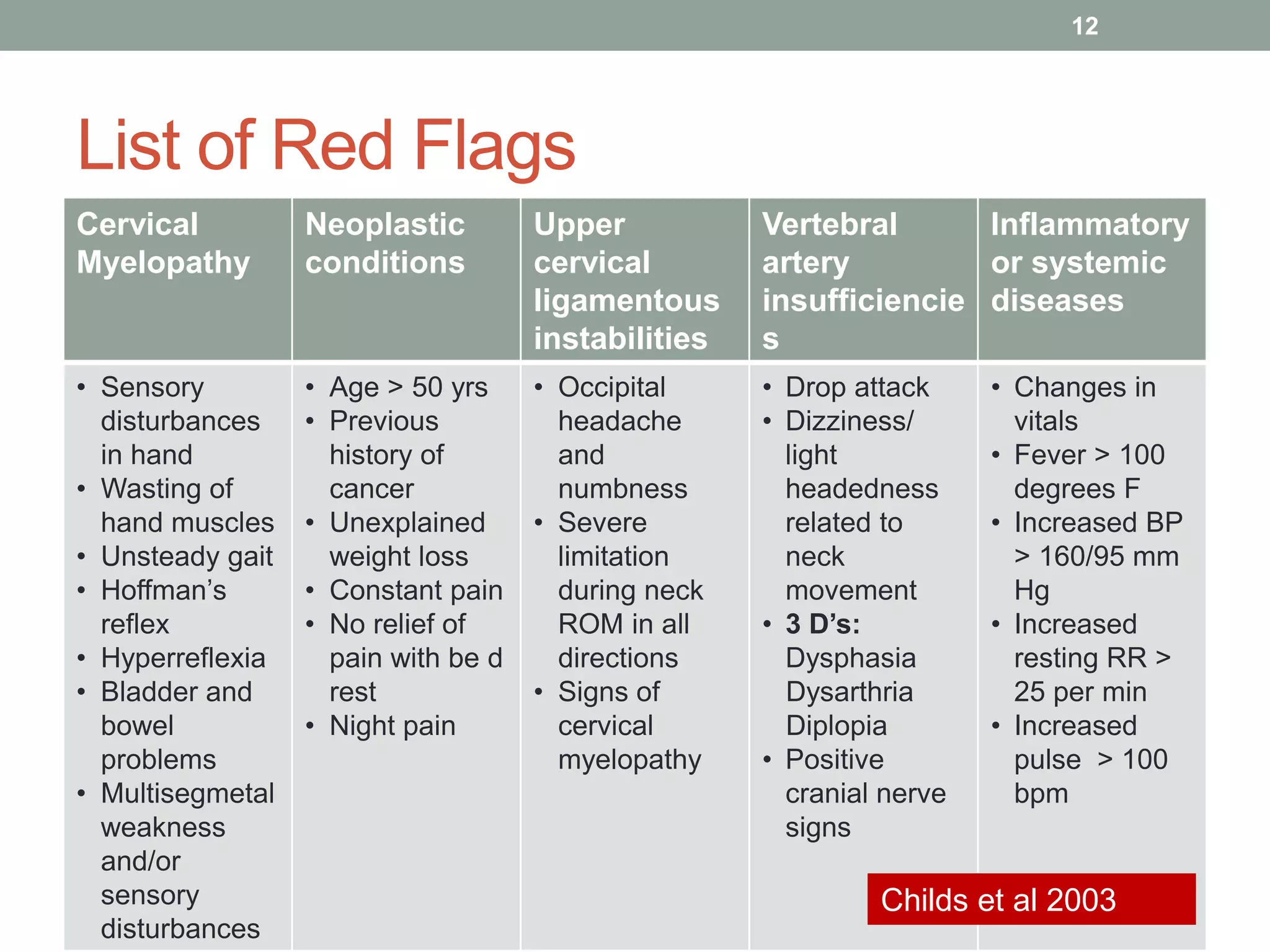
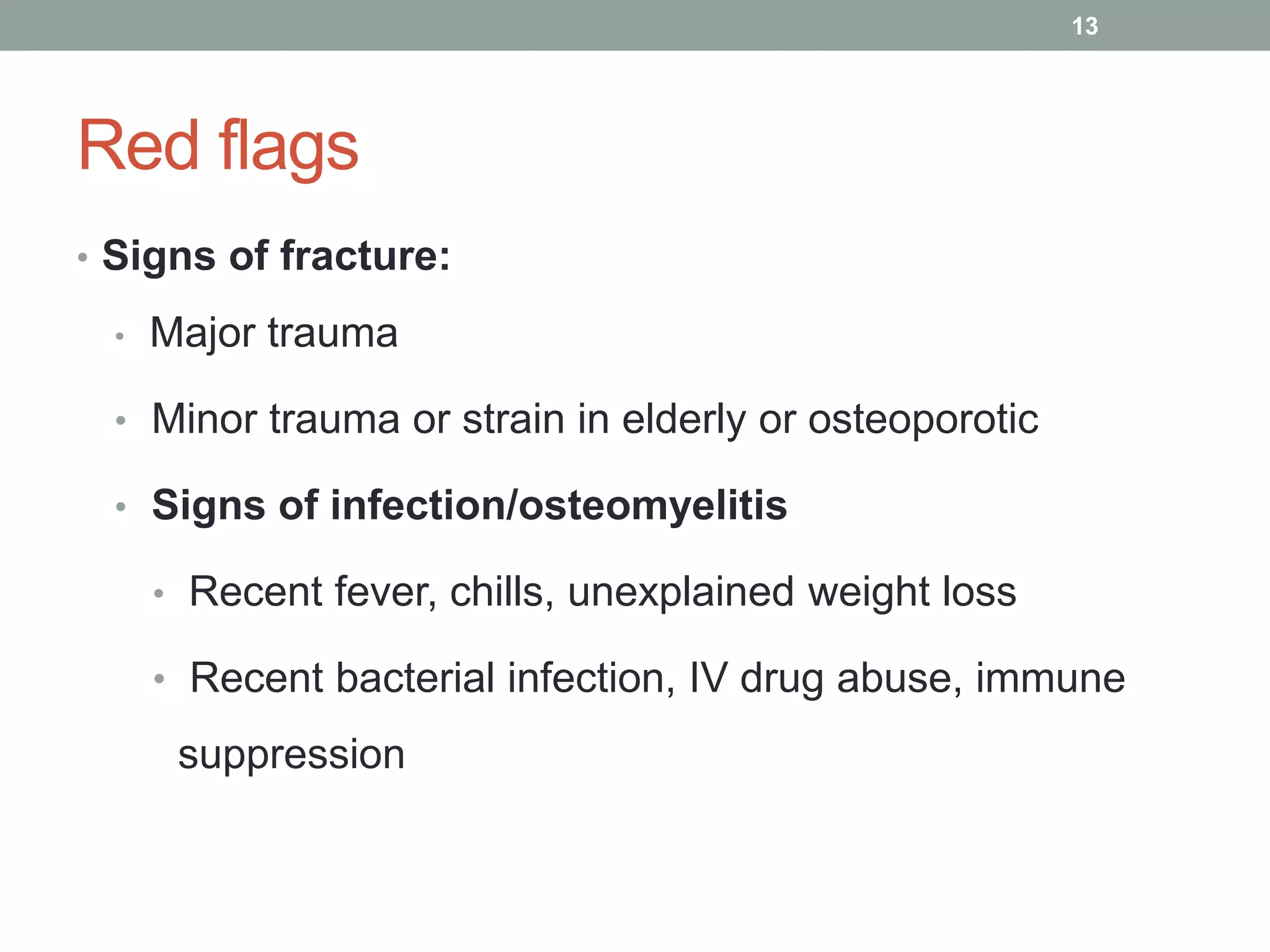
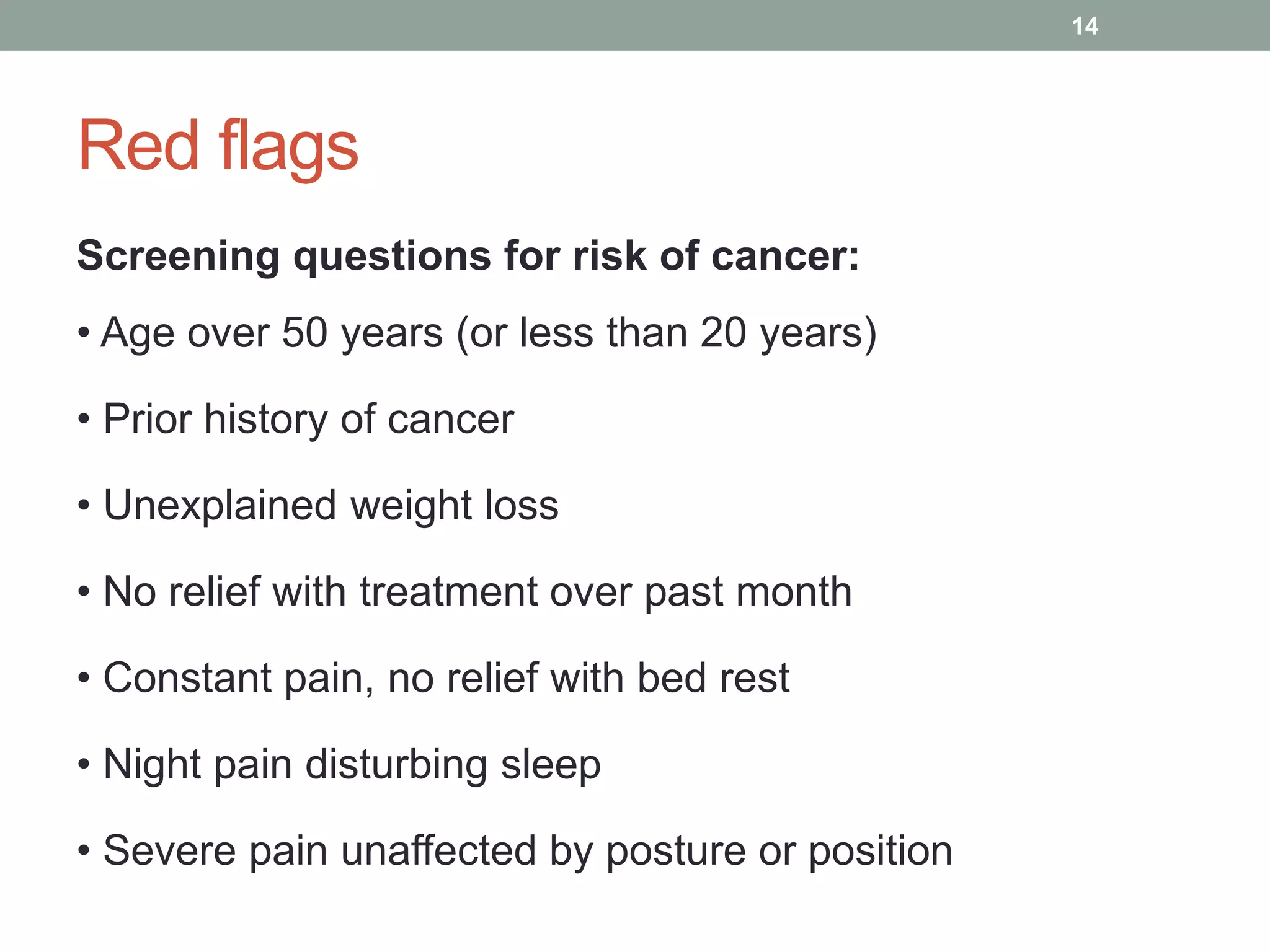
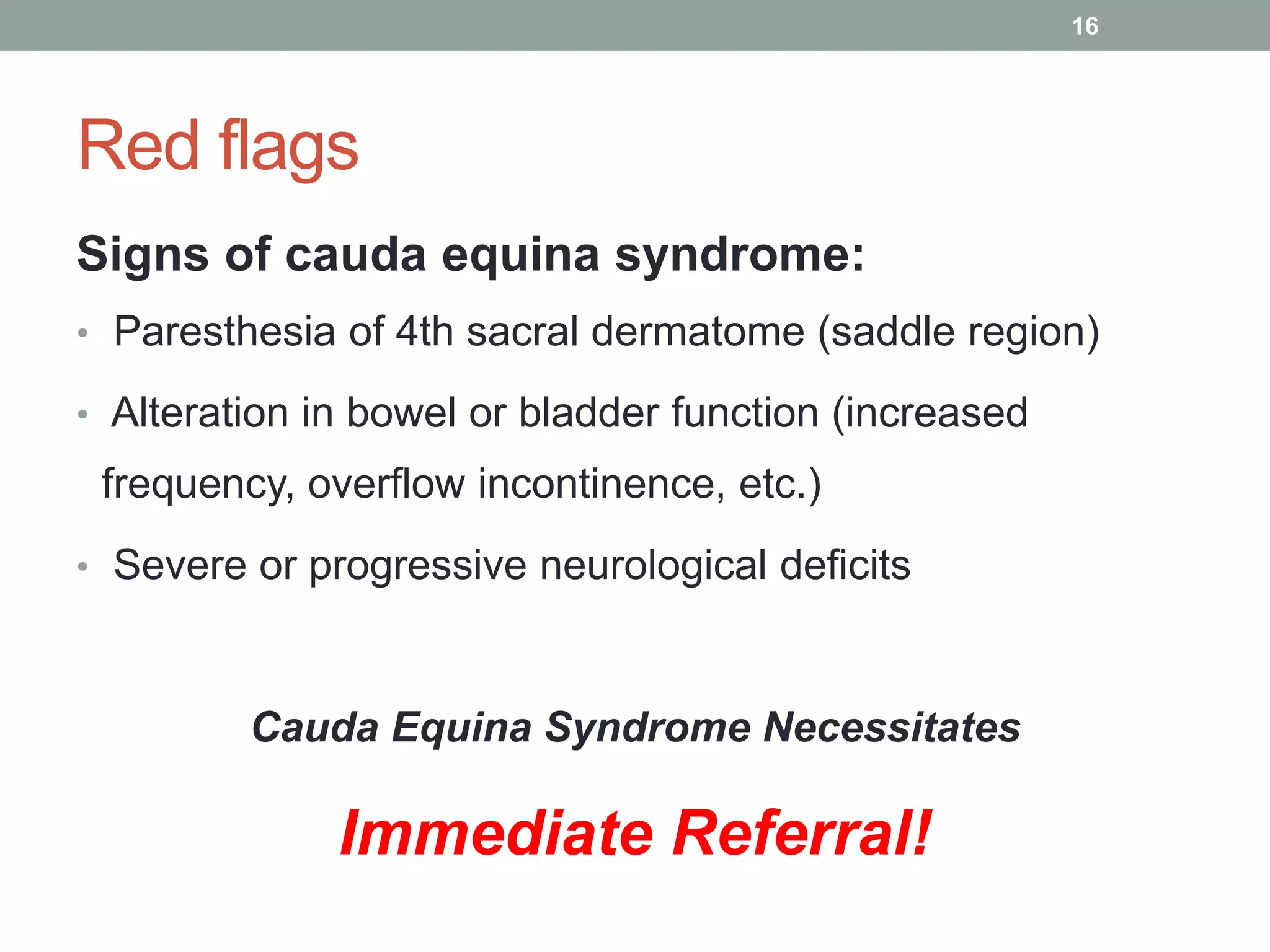
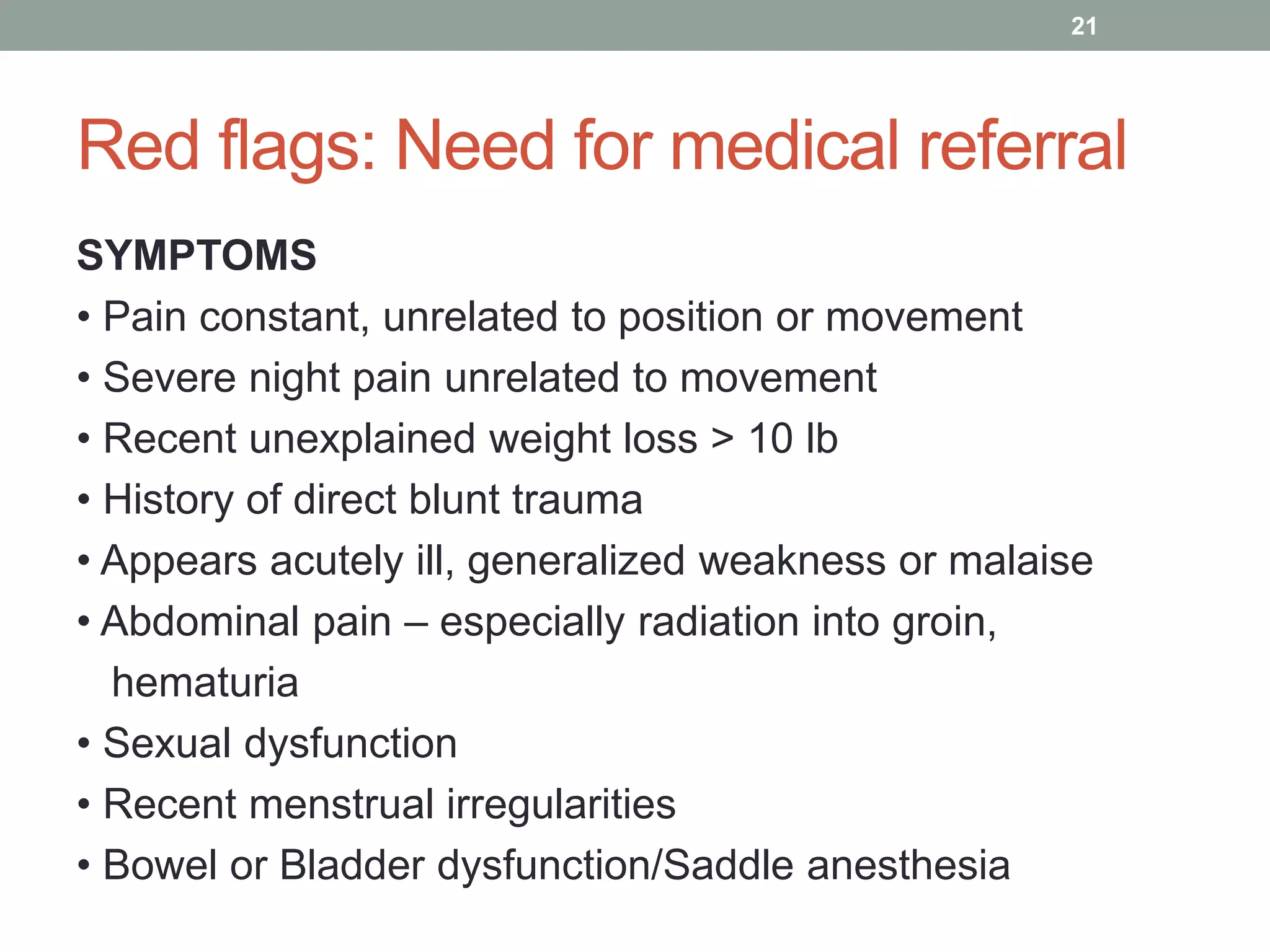
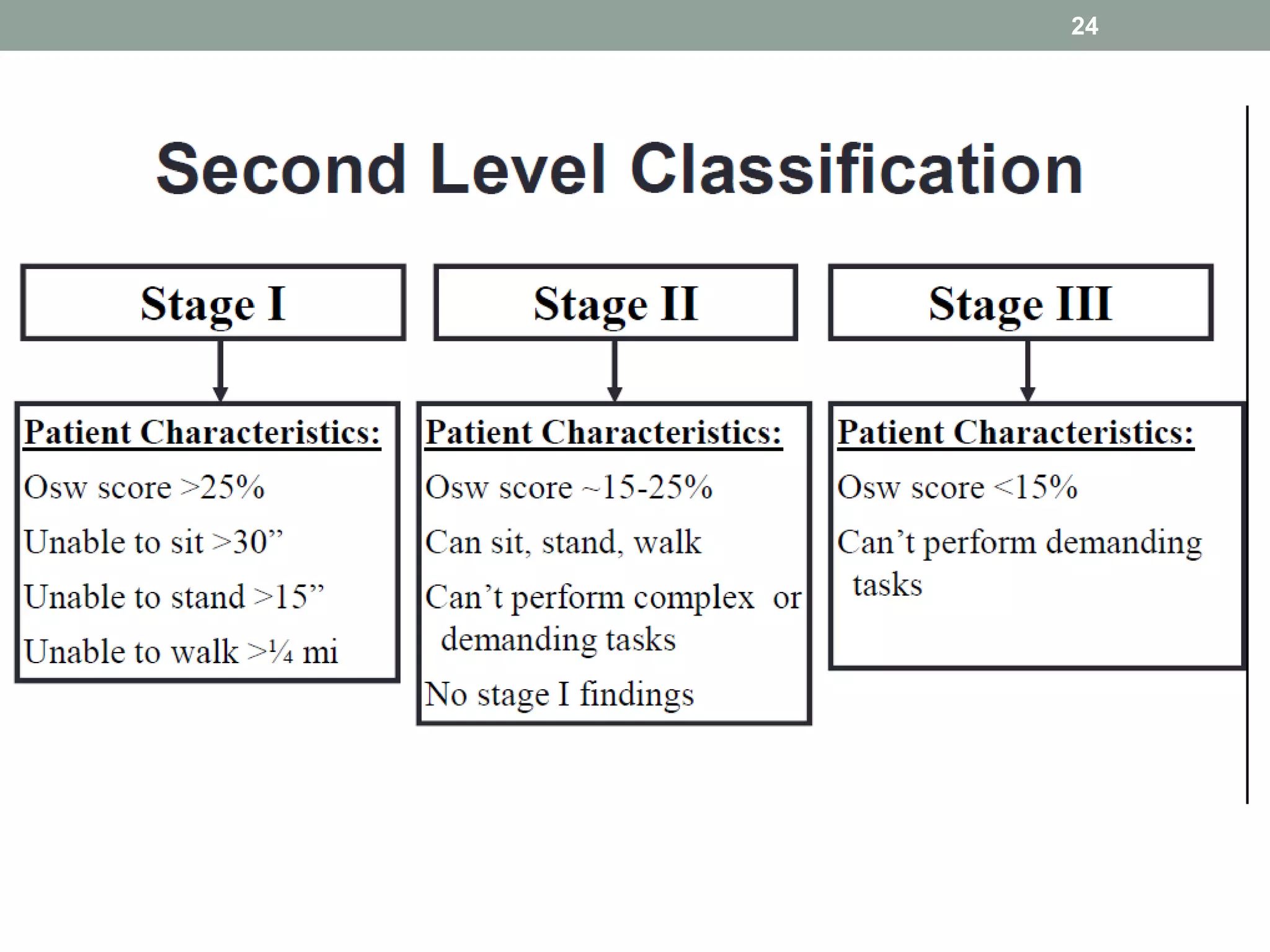
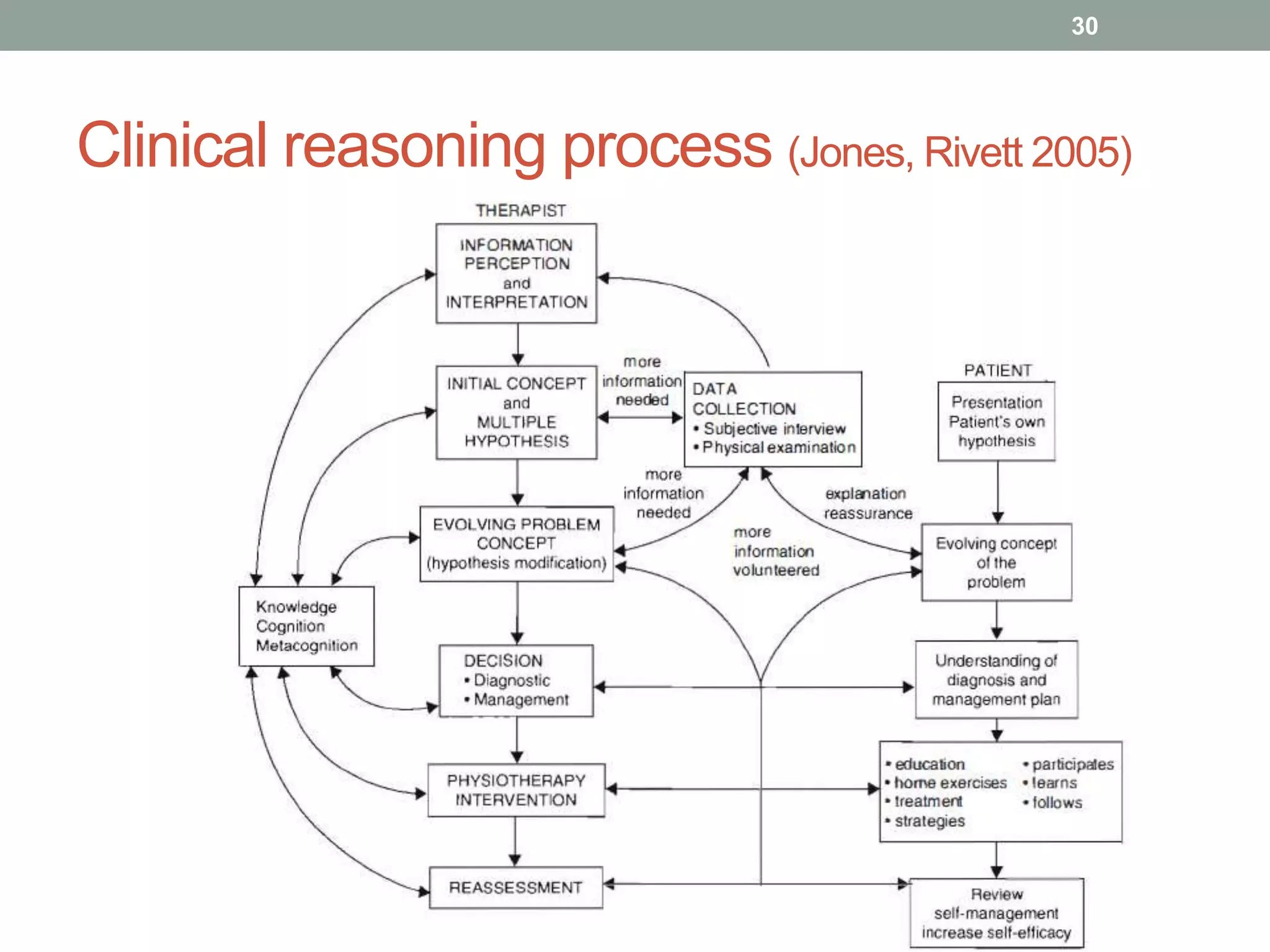
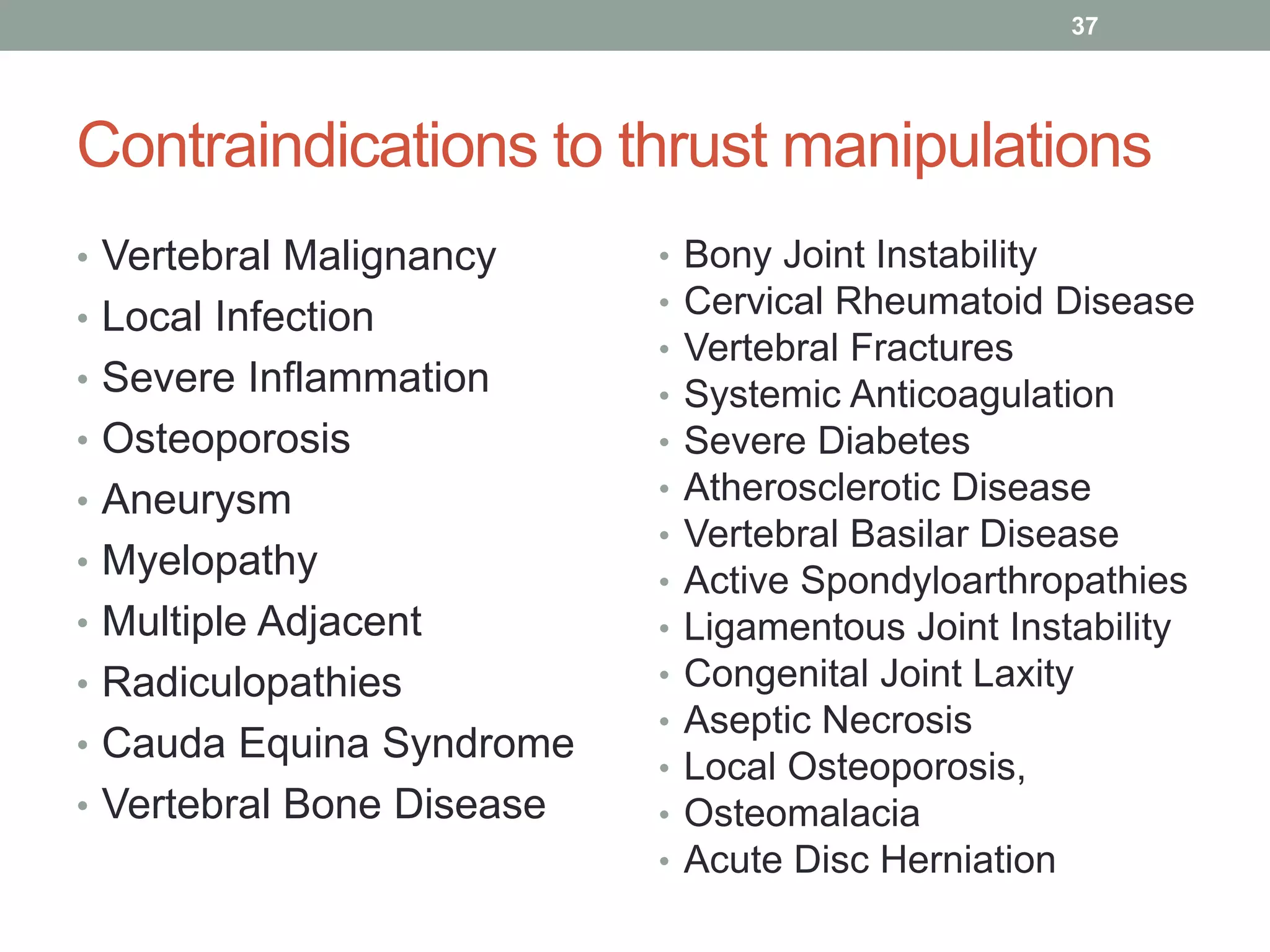
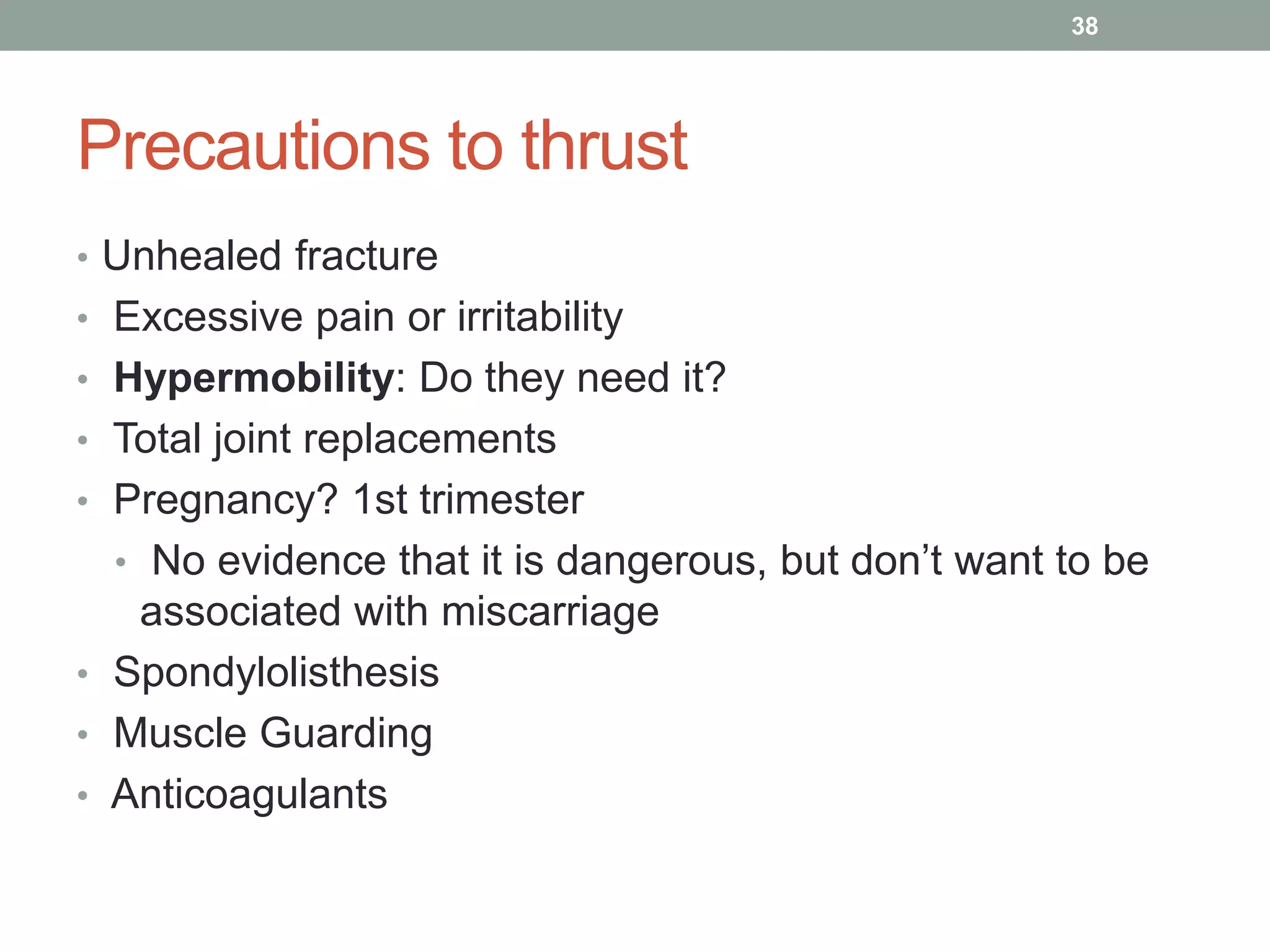
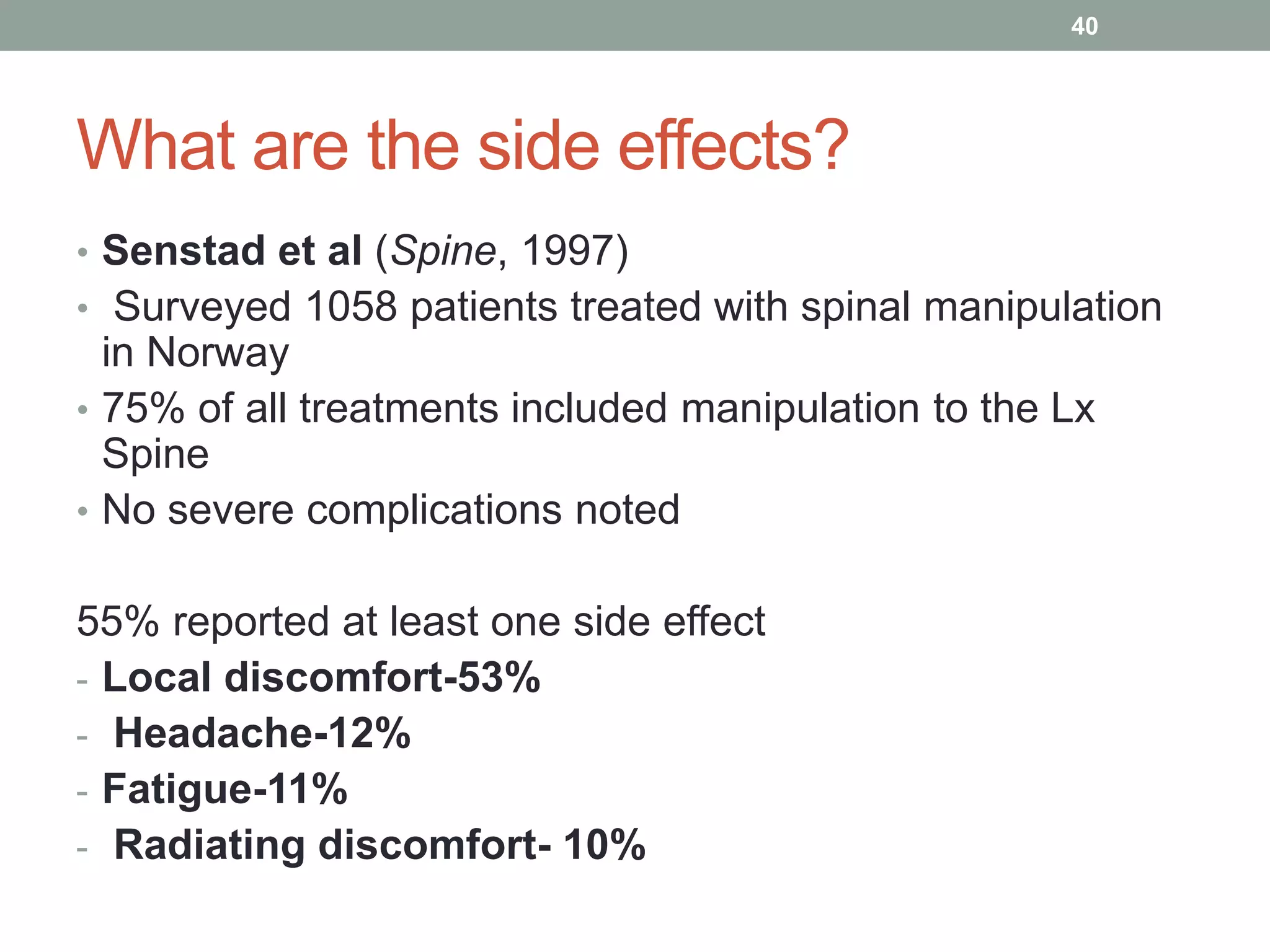
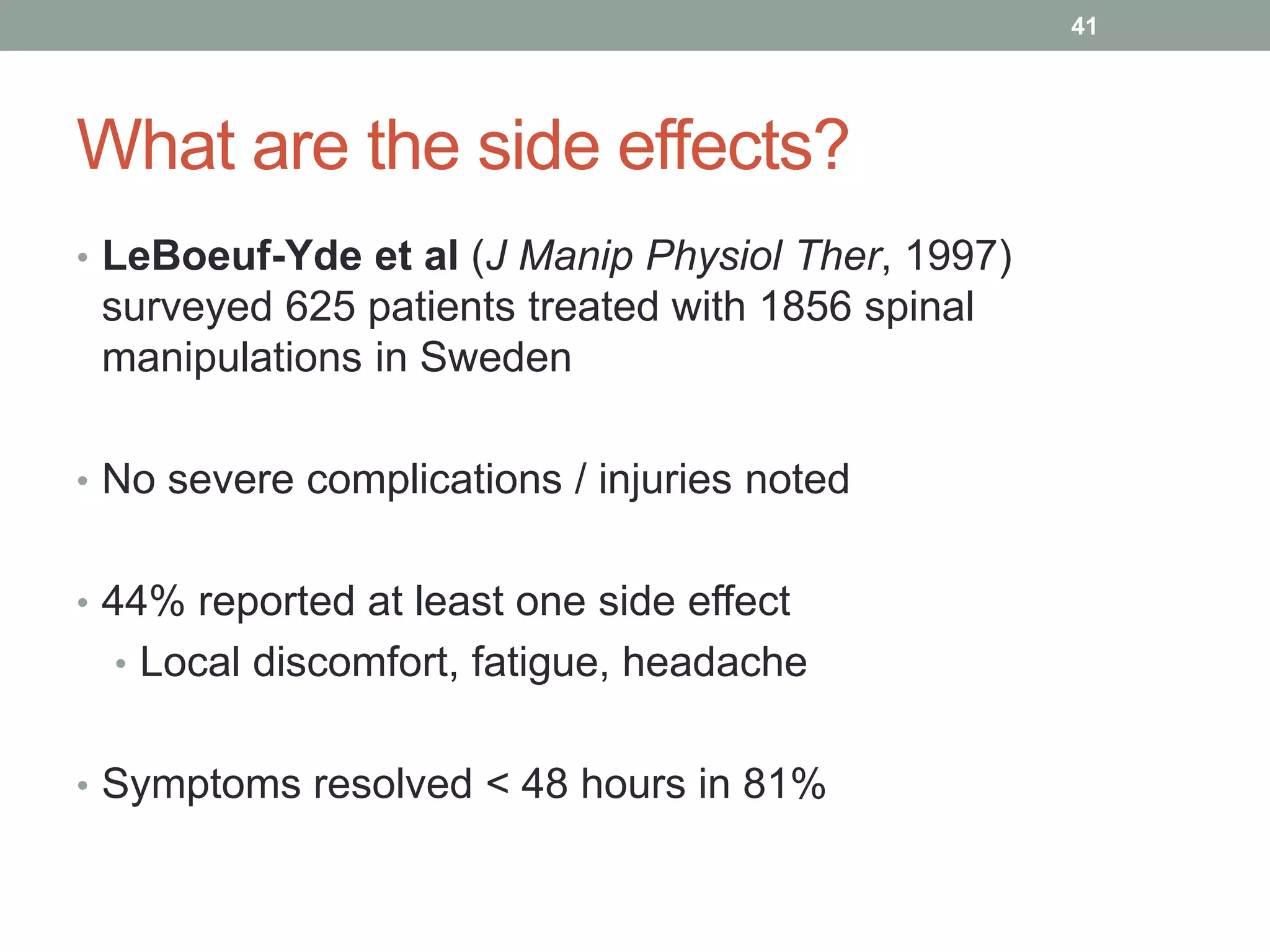
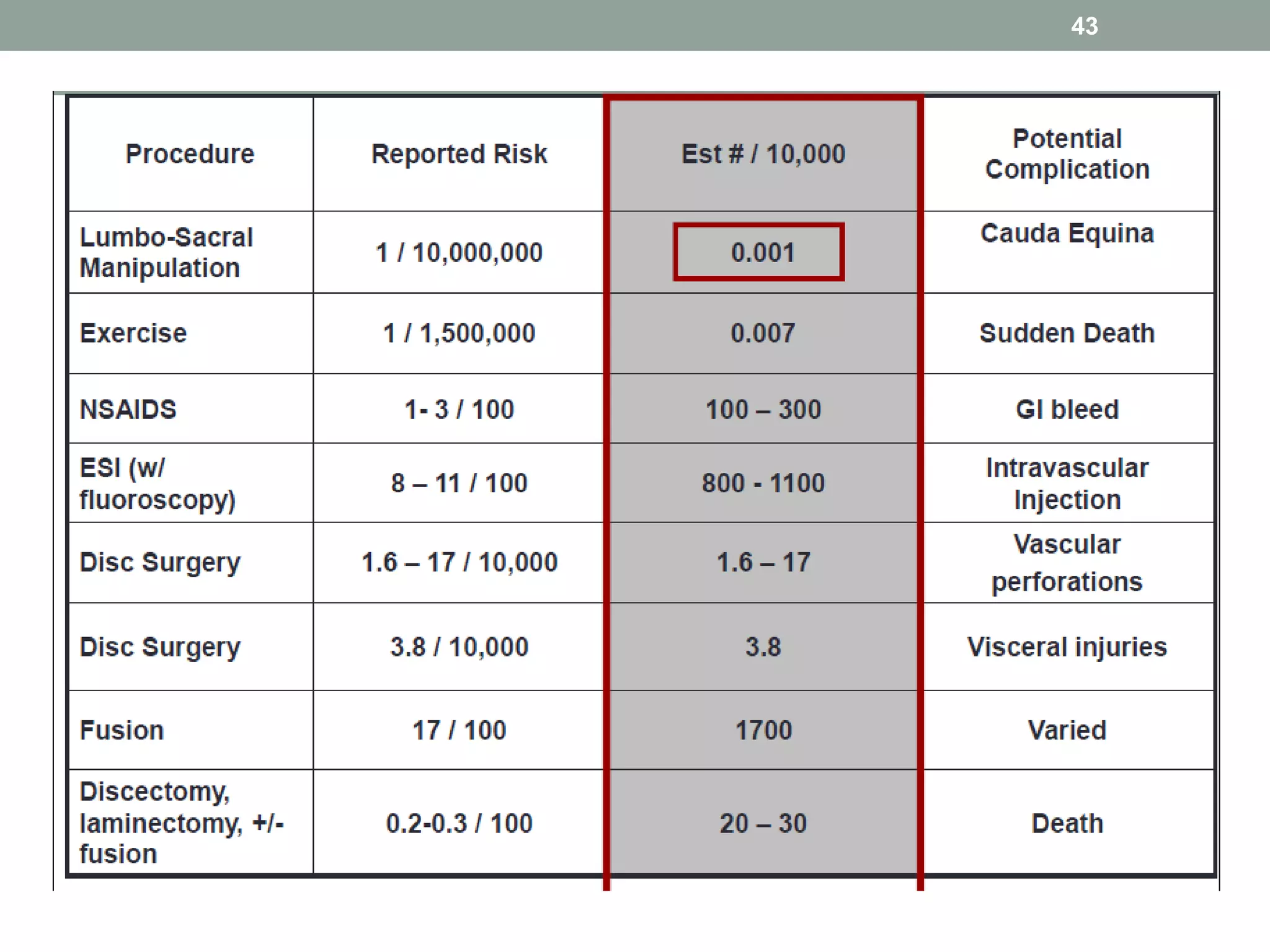
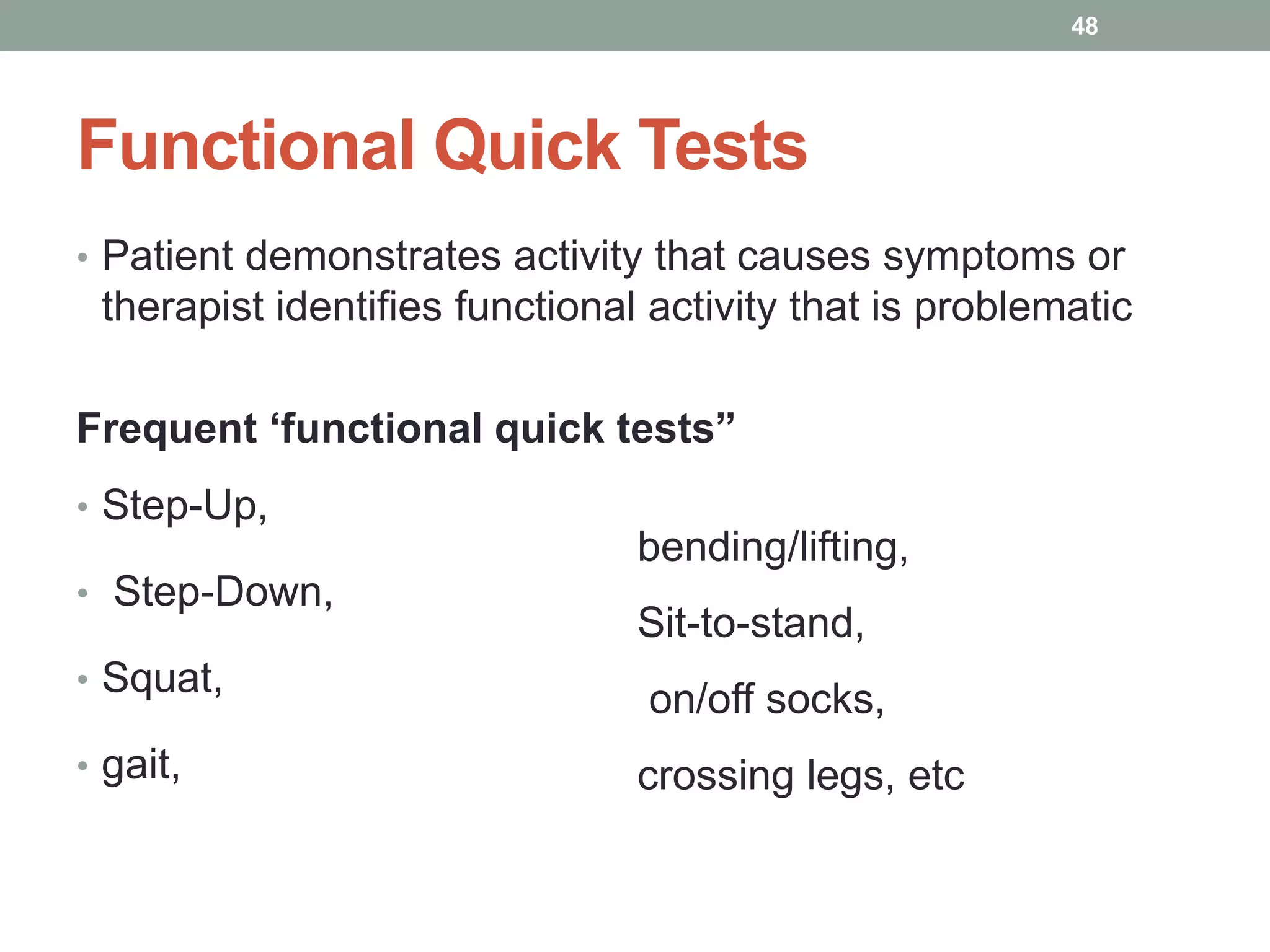
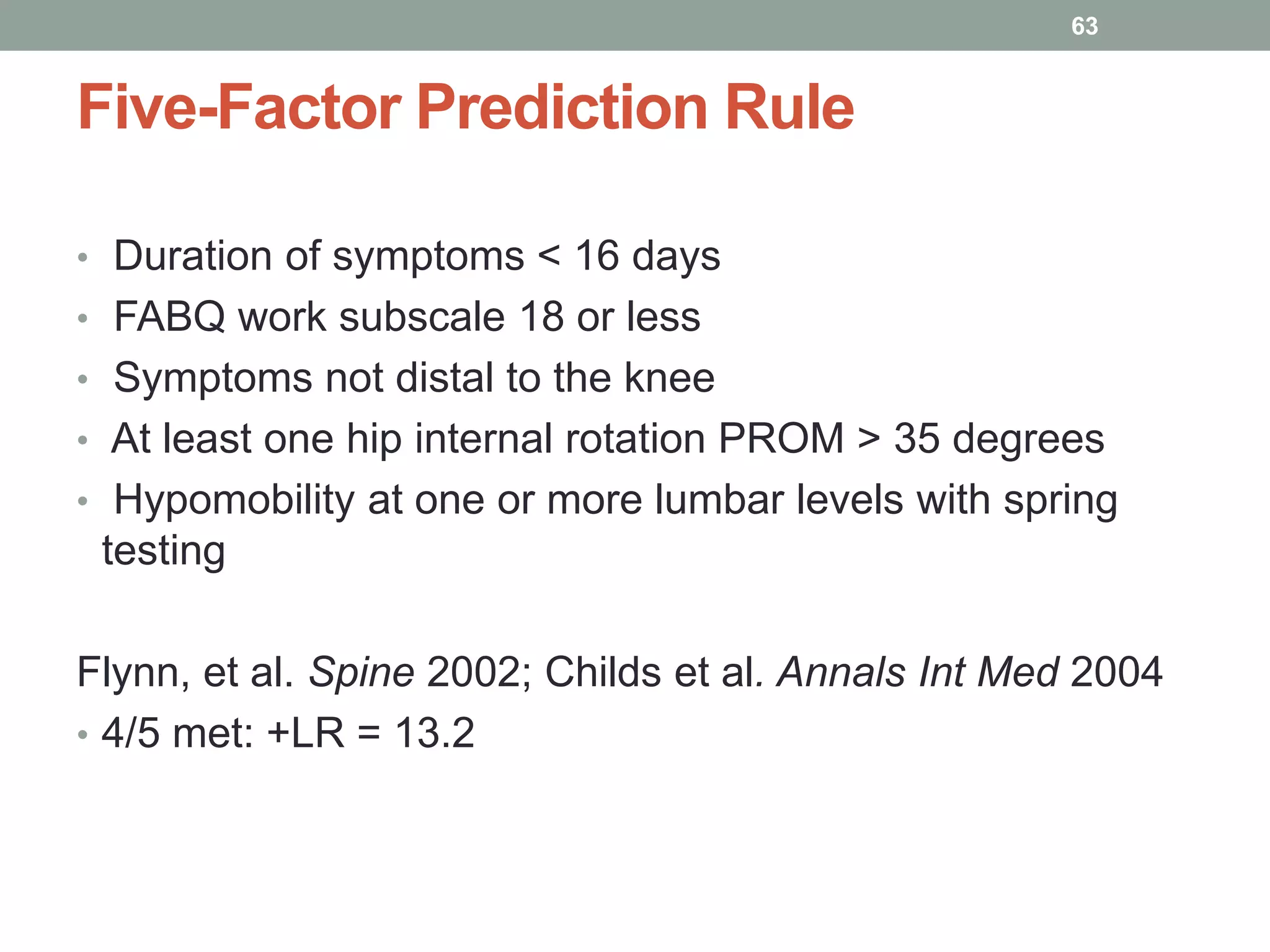
This document outlines the principles and practices of manipulation in physiotherapy, including assessment methods, indications, contraindications, and treatment classification. It emphasizes the importance of a thorough patient history and objective assessment in determining suitability for manipulation and highlights key red and yellow flags that necessitate referral. The document also discusses various mobilization techniques, risks associated with manipulation, and the importance of clinical reasoning throughout the treatment process.