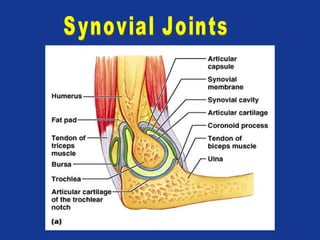
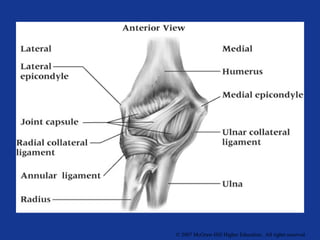
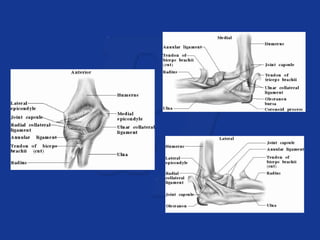
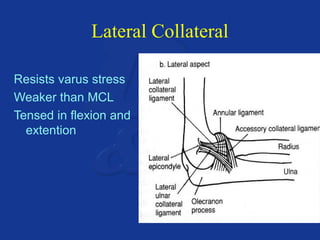
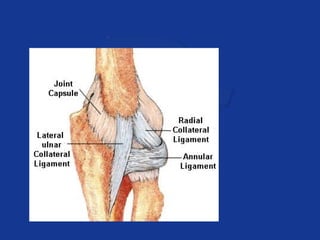
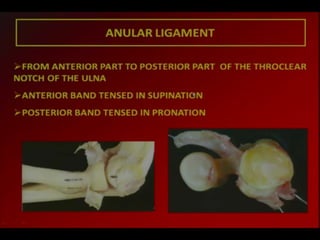
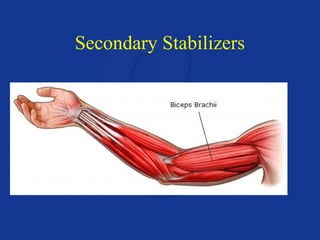
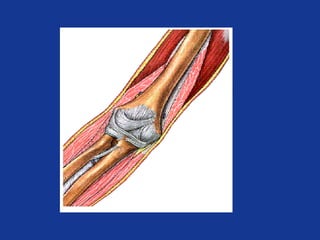
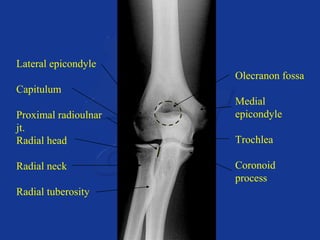
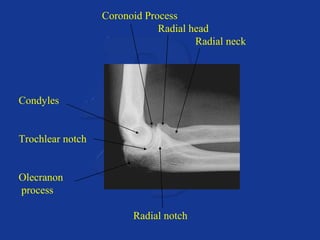
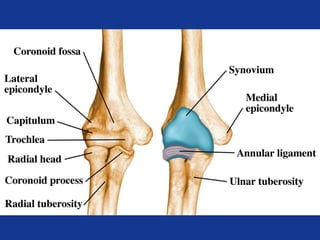
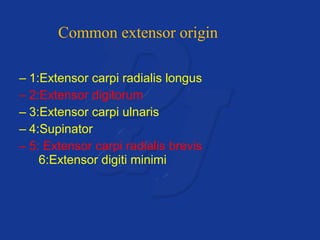
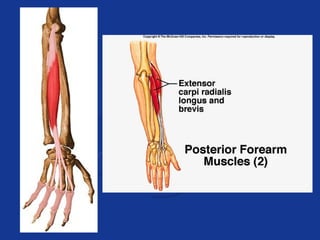
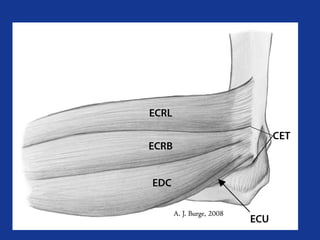
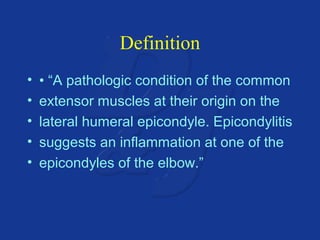
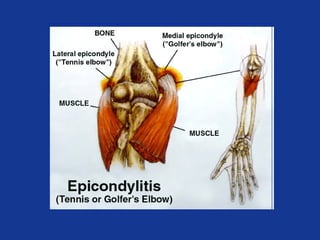
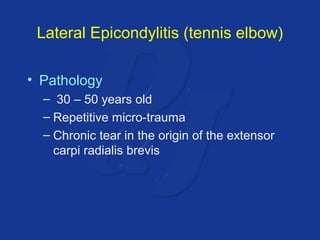
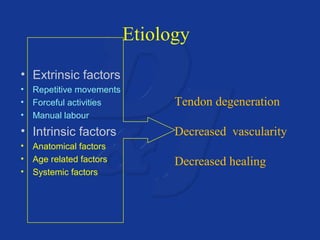
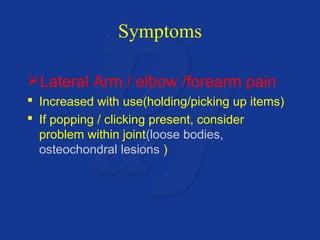
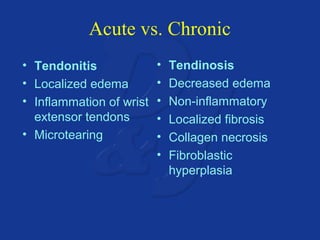
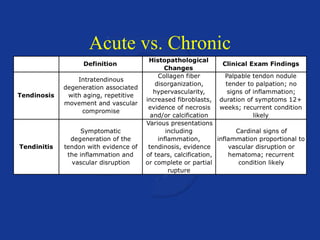
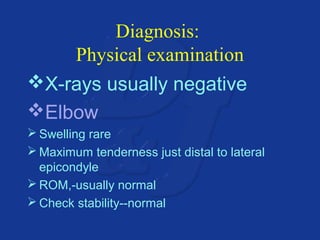
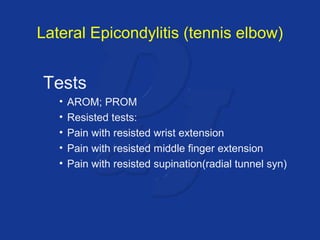
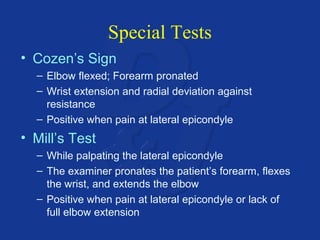
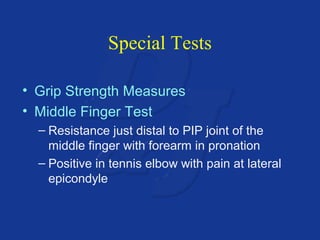
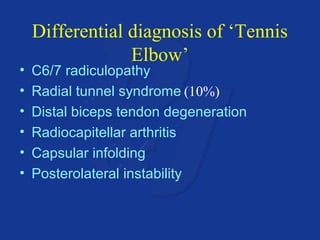
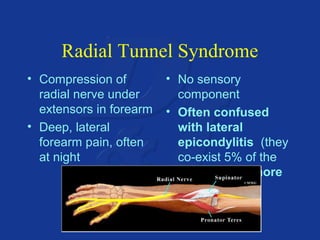
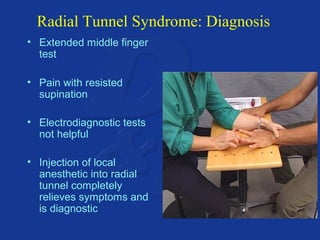
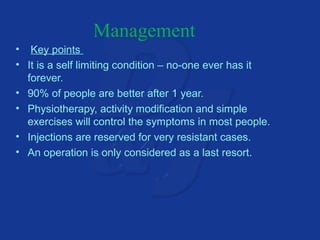
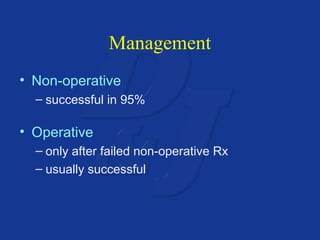
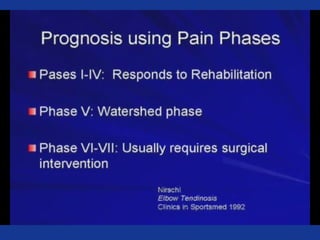
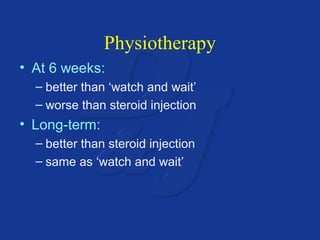
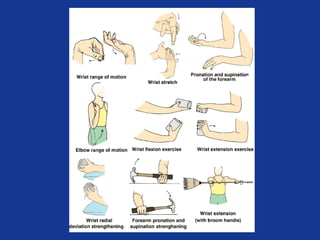
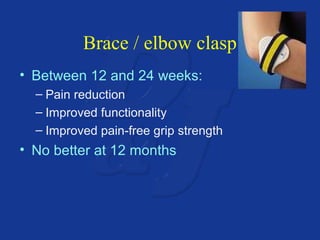
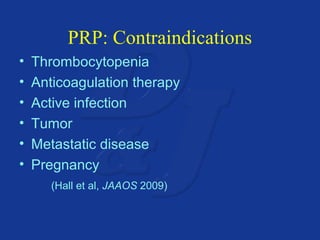
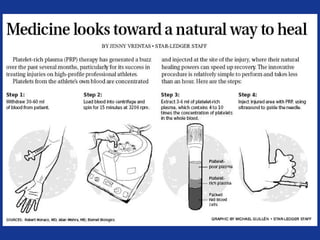
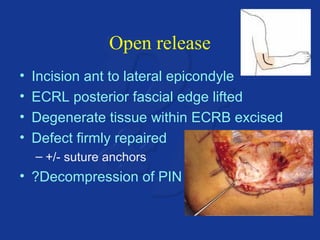
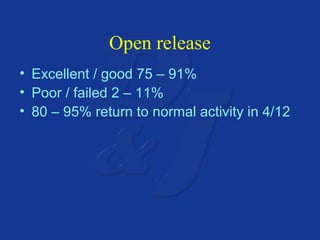
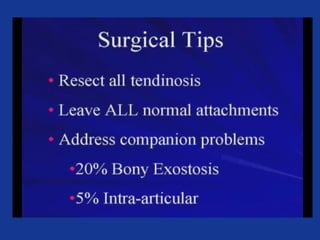
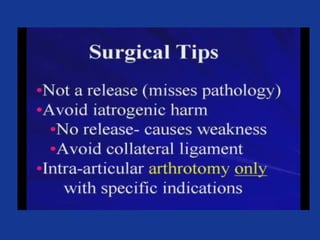
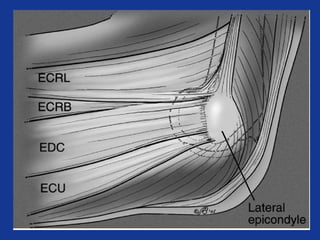
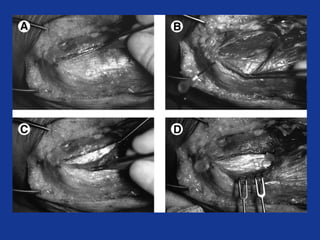
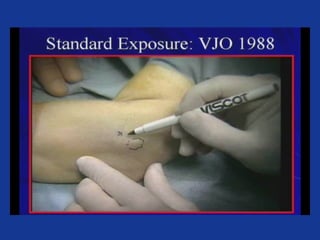
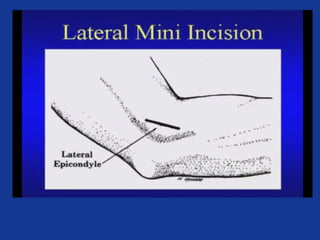
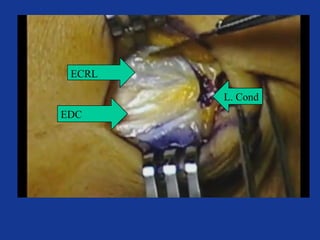
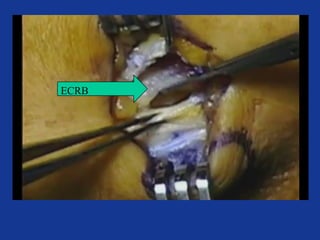
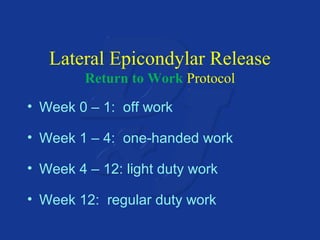
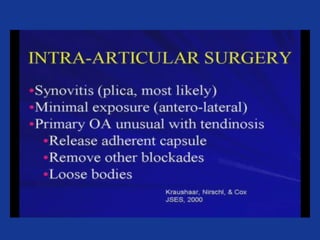
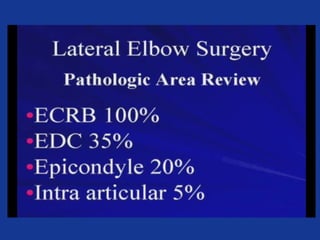
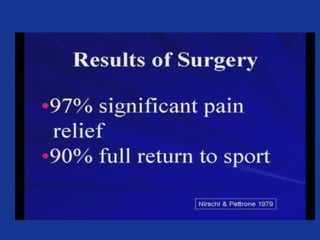
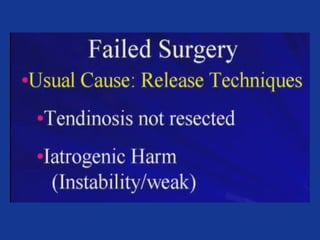
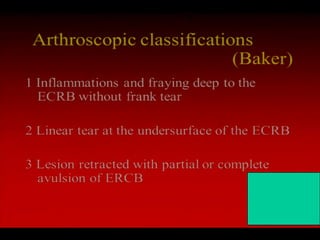
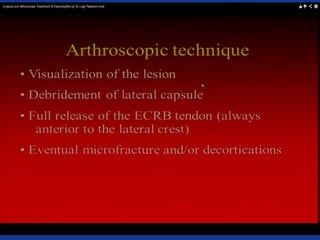
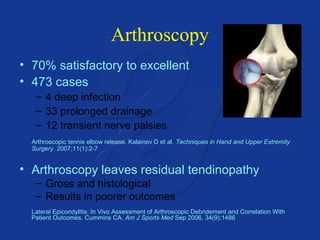
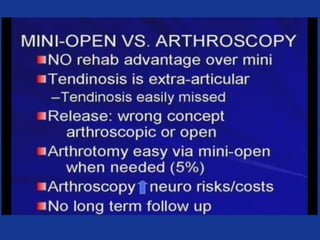
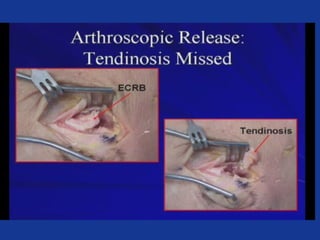
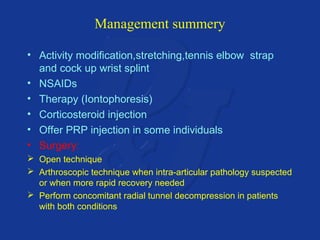
This document provides information on lateral epicondylitis (tennis elbow), including its anatomy, causes, symptoms, diagnosis, and treatment options. It describes how lateral epicondylitis is an overuse injury caused by repetitive microtrauma to the common extensor tendon at the lateral epicondyle. The diagnosis is typically made based on physical examination findings of tenderness over the lateral epicondyle with resisted wrist and finger extension. Both non-operative treatments like physiotherapy, bracing, and steroid injections and surgical options are discussed for managing lateral epicondylitis.