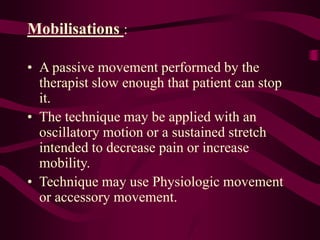
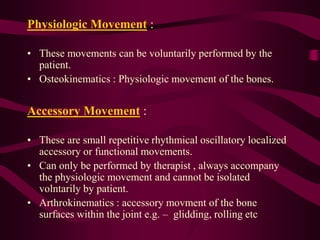
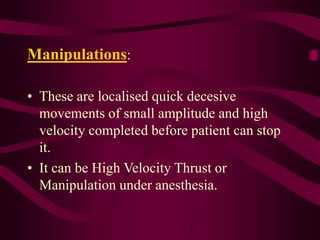
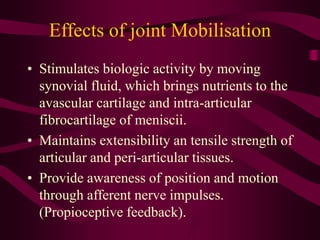
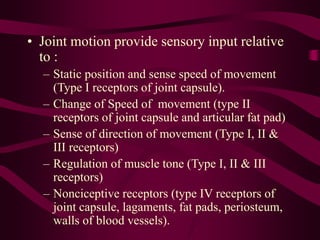
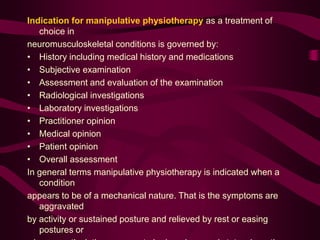
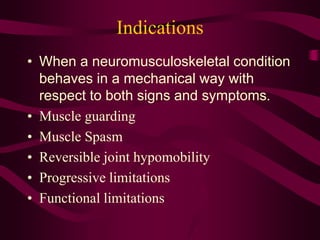
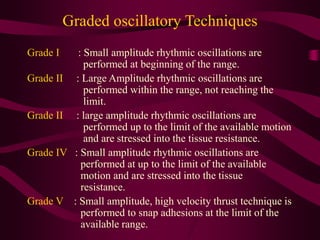
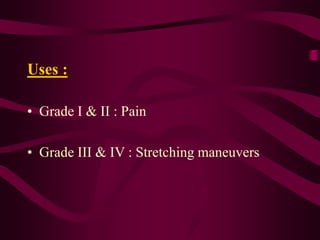
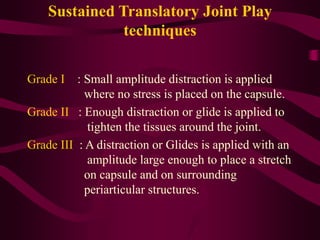
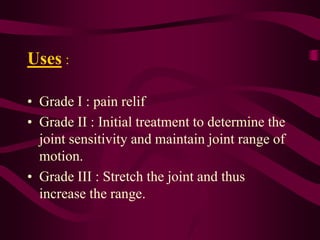
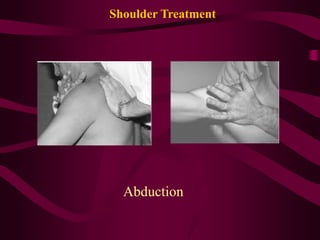
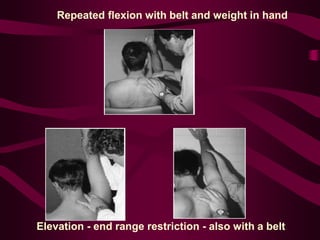
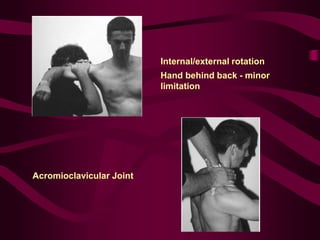
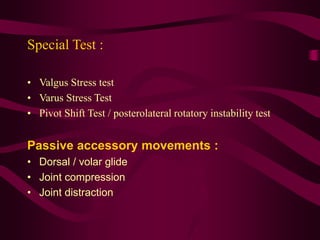
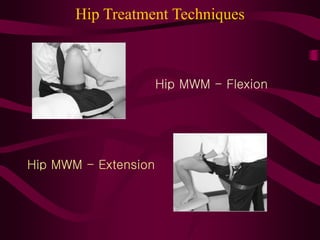
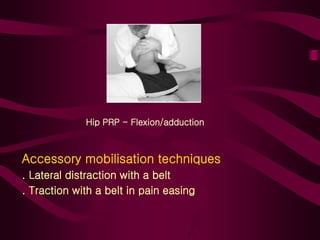
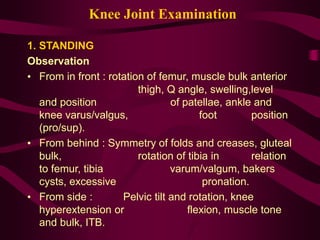
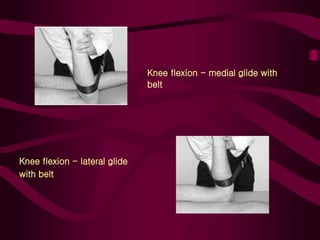
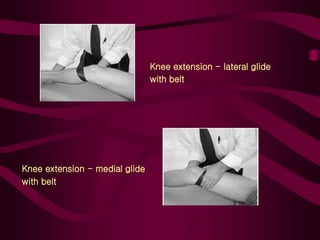
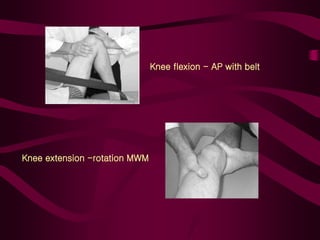
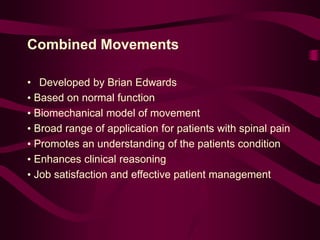
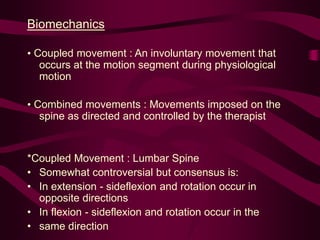
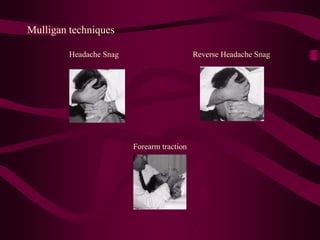
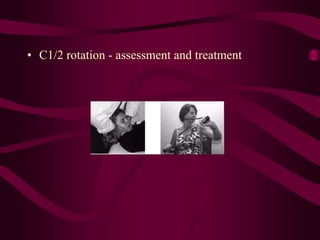
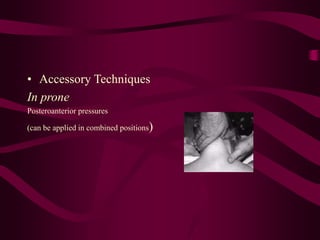
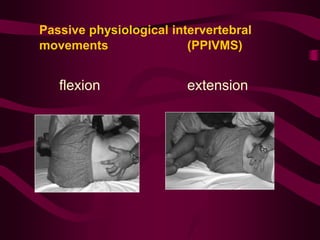
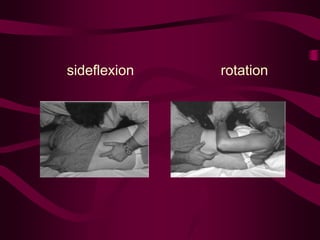
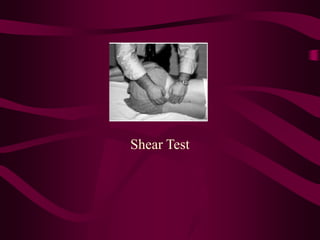
Manual therapy techniques like joint mobilizations and manipulations can be used to safely restore normal joint mechanics and reduce trauma. Effective use requires knowledge of anatomy, arthrokinematics, and pathologies. Several concepts for manual therapy techniques were introduced, including Cyriax, Mulligan, Maitland, and McKenzie. Contraindications include inflammation, effusion, and hypermobility while indications include reversible hypomobility and functional limitations responding to mechanical treatment. Grading systems determine appropriate mobilization force and different joints require specific examination and treatment techniques.