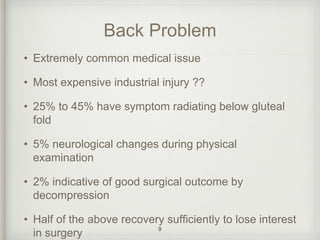
This document discusses lumbar pain and low back pain. Some key points:
- Low back pain is very common, expensive, and a leading cause of disability.
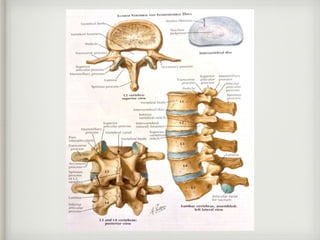
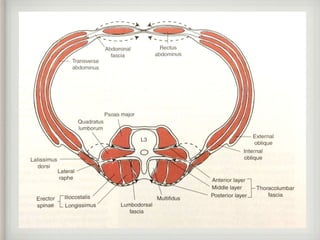
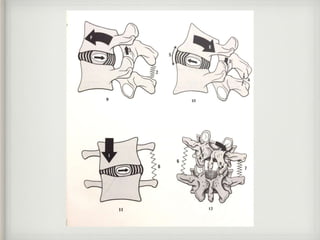
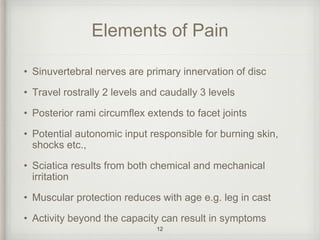
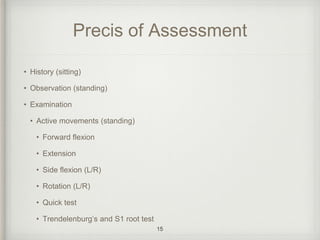
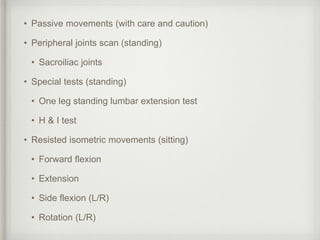
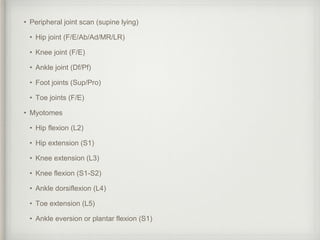
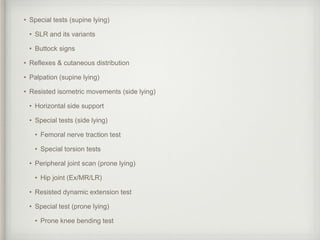
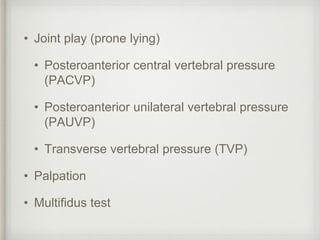
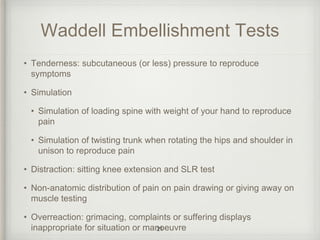
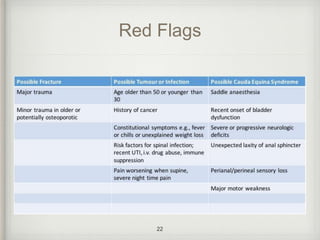
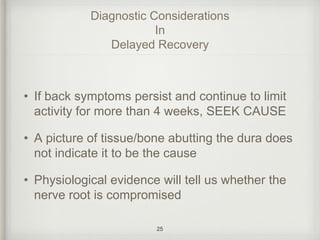
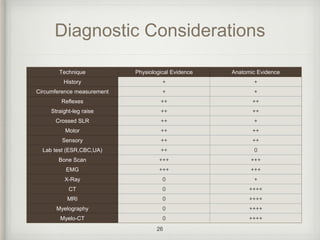
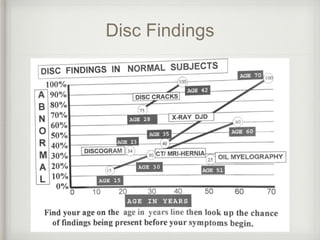
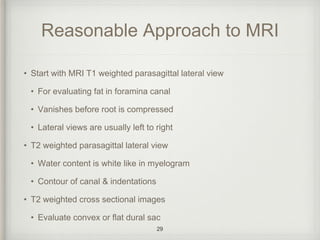
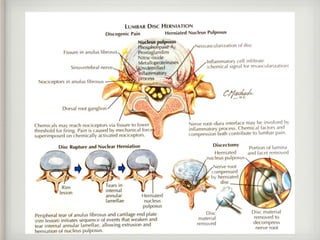
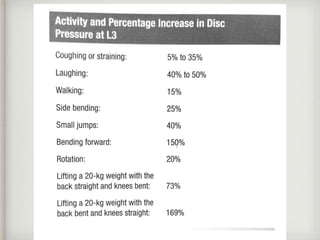
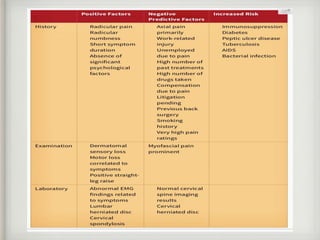
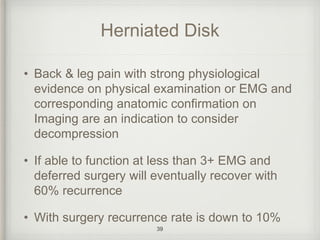
- Physical examination and imaging tests can help evaluate the source and severity of back pain.
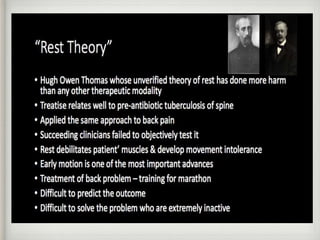
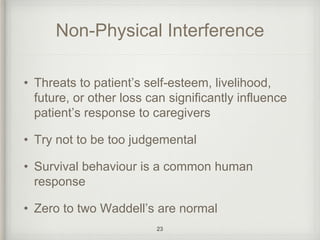
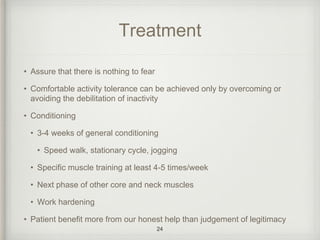
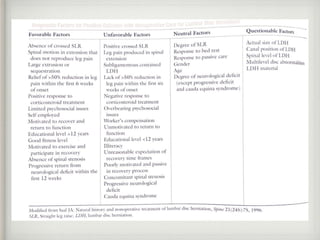
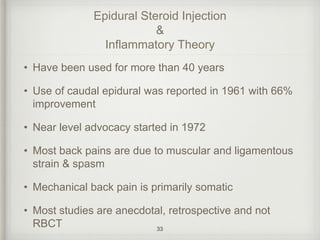
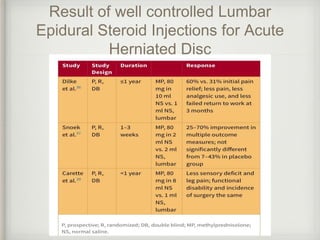
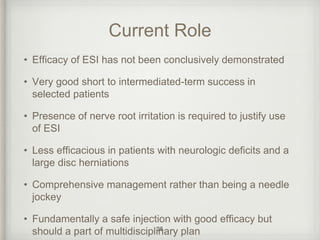
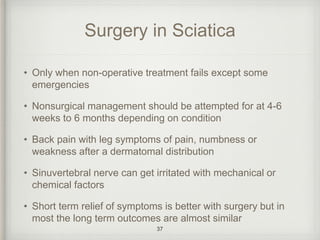
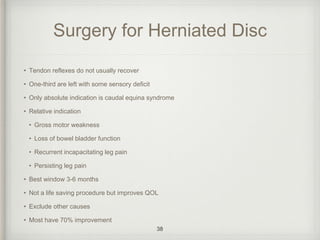
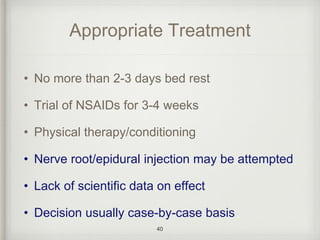
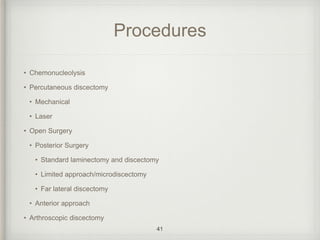
- Treatments may include exercise, medication, injections, and in some cases surgery. However, surgery outcomes are often similar to non-surgical treatments.
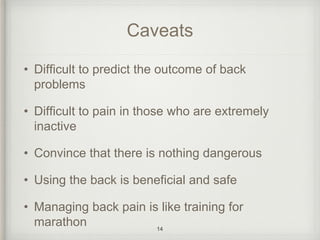
- Proper diagnosis is important to guide treatment, as many cases of back pain resolve on their own with time and conservative care.