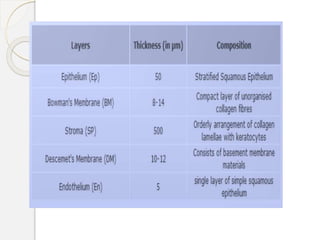
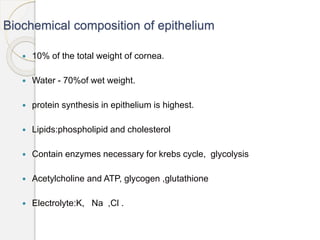
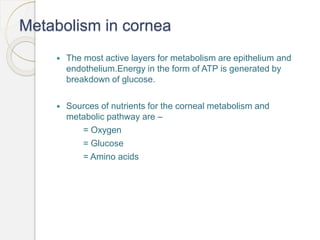
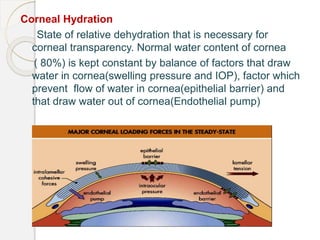
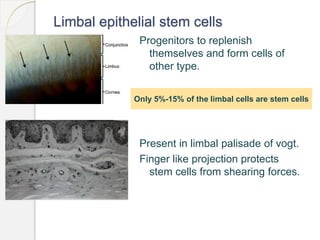
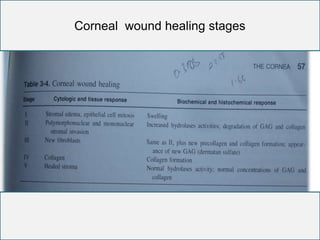
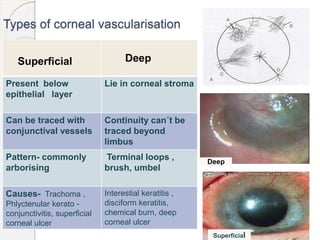
The document provides information on the physiology and biochemistry of the cornea. It discusses the cornea's structure, composition, function, metabolism, wound healing, and factors that affect transparency. The cornea's layers are composed primarily of water, collagen, and proteoglycans. It maintains transparency through its regular stromal spacing and metabolic pumps that regulate hydration. The cornea relies on limbal stem cells and tight epithelial/endothelial barriers to replenish and prevent edema.