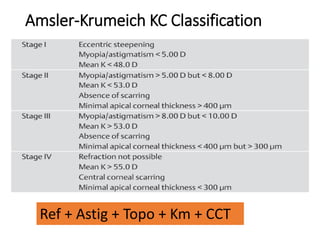
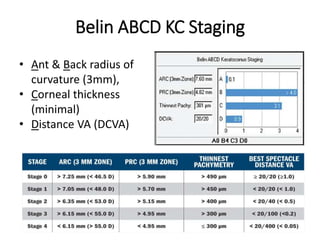
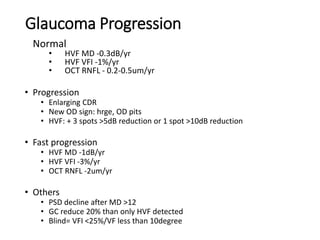
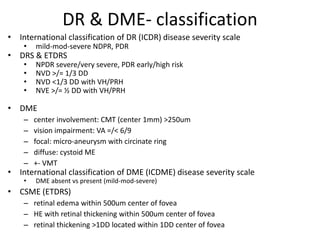
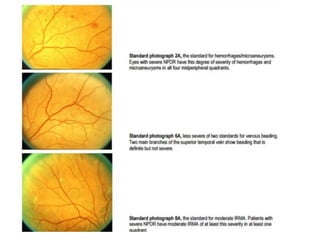
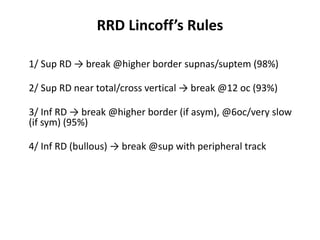
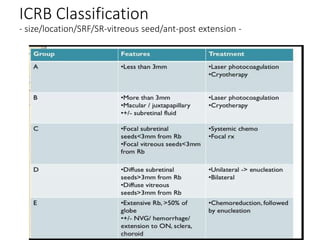
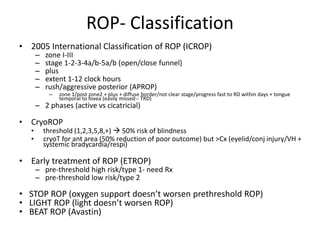
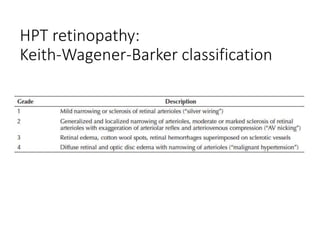
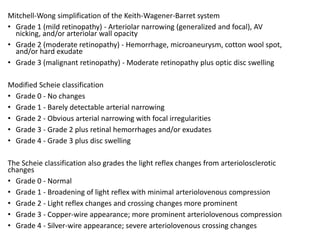
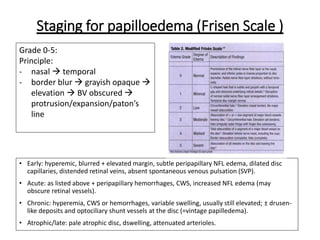
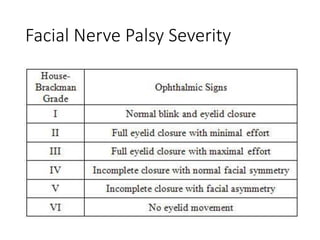
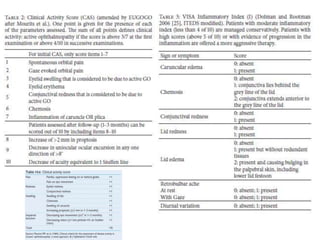
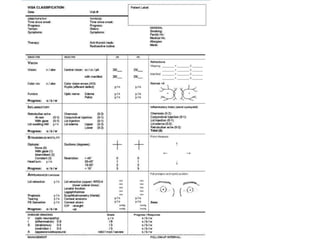
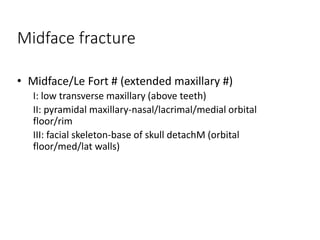
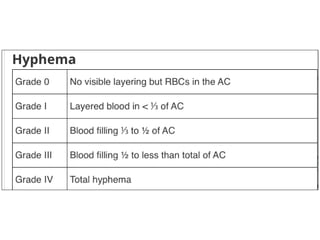
This document discusses various classification and staging systems used in ophthalmology. It covers classifications for corneal and external eye diseases, glaucoma, uveitis, vitreo-retinal diseases, and others. For each condition, it provides details on the classifications used to describe risk factors, pathogenesis, clinical features, severity, investigations, and management approaches. The classifications discussed include international standardized systems as well as other commonly used staging methods.