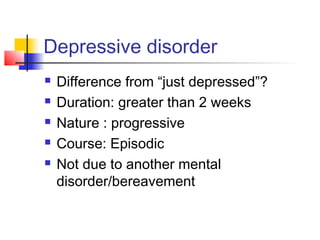
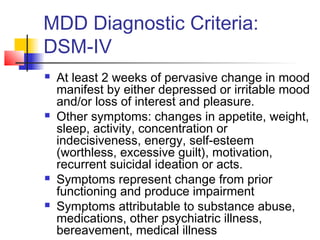
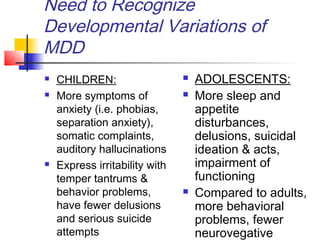
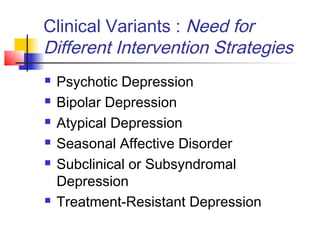
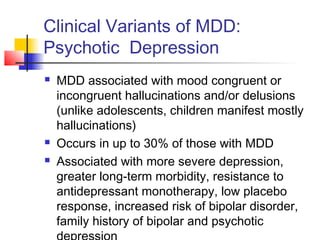
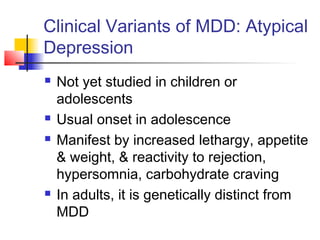
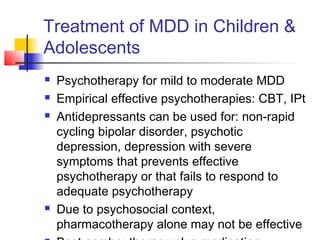
This document discusses depressive disorders in children and adolescents. It defines major depressive disorder and notes key diagnostic criteria including a change in mood and impairment lasting at least two weeks. Developmental variations are important to recognize, as children may show more irritability and somatic complaints while adolescents have more sleep, appetite issues and suicidal thoughts. Properly diagnosing and treating depressive disorders in young people can be challenging due to developmental factors and complexity. Theories around causes include psychological, biological and environmental influences. Clinical variants like psychotic depression require different treatment strategies, and both psychotherapy and antidepressants may be used depending on severity.