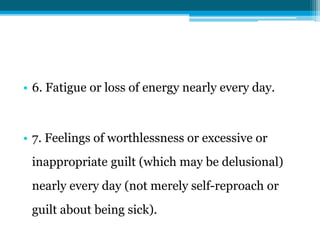
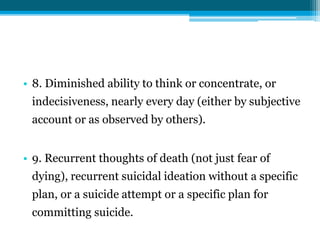
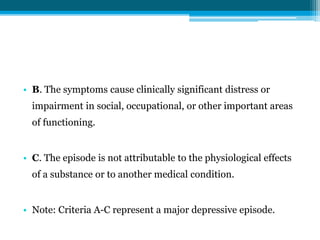
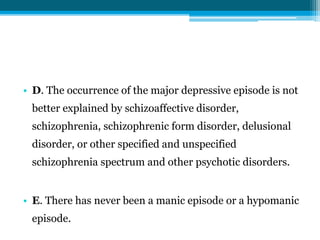
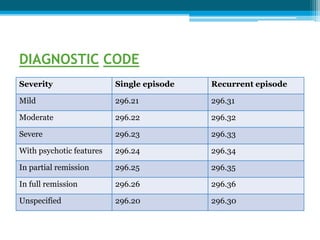
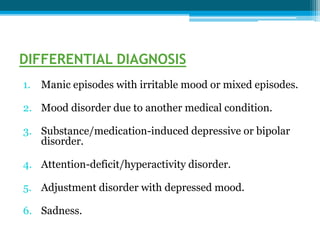
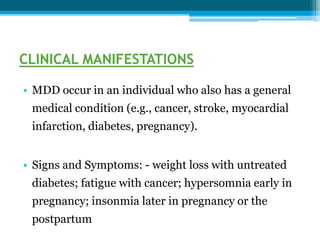
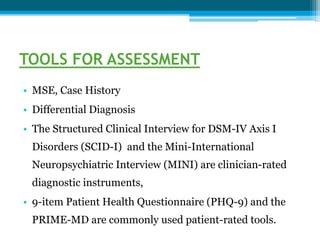
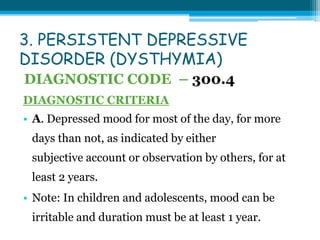
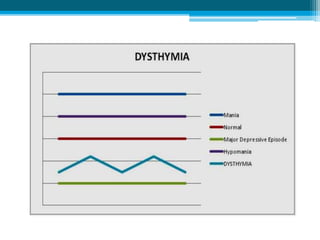
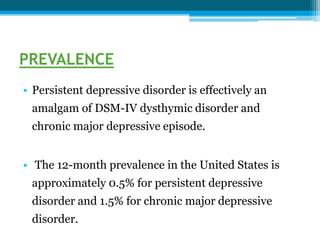
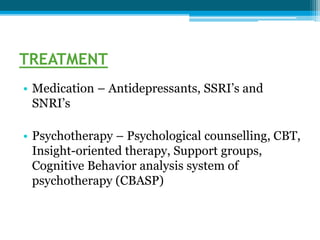
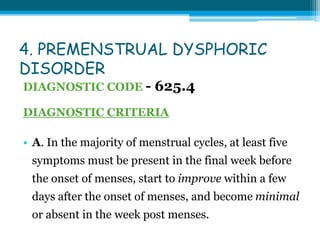
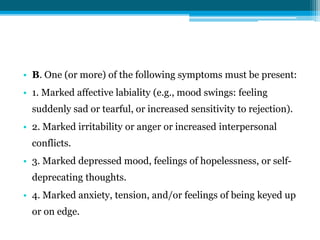
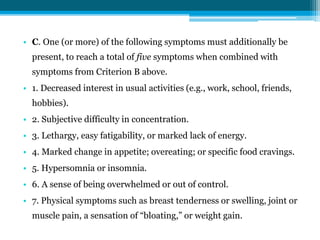
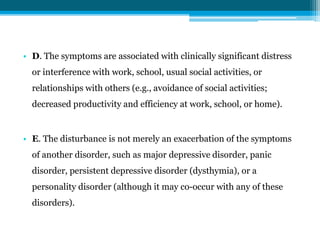
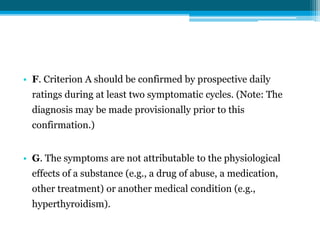
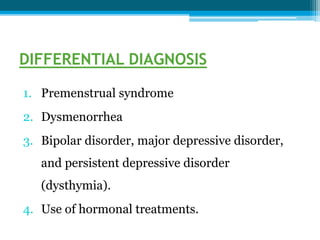
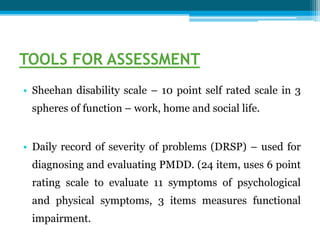
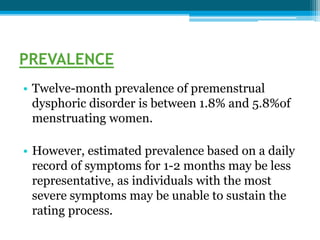
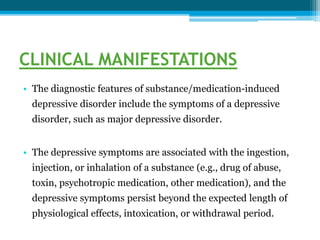
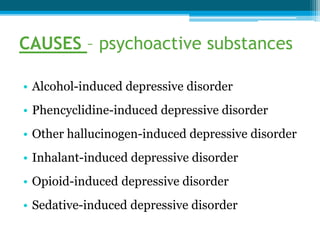
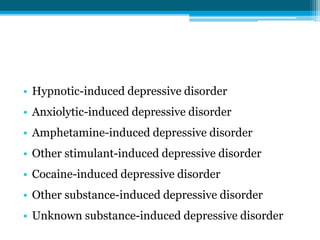
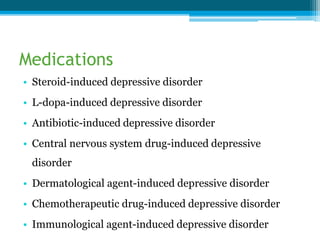
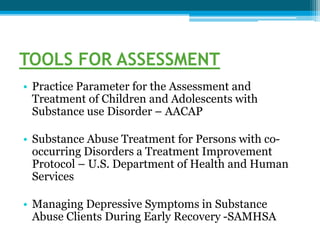
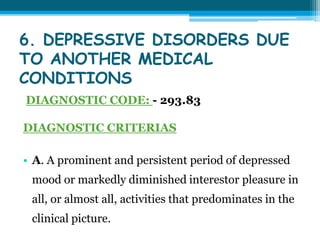
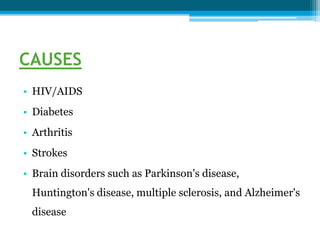
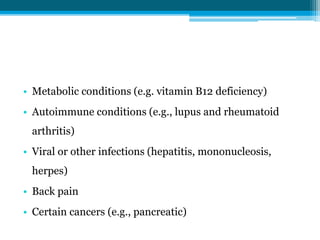
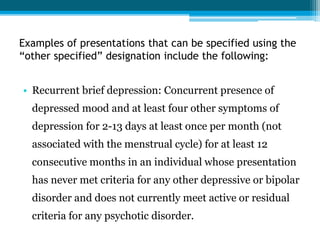
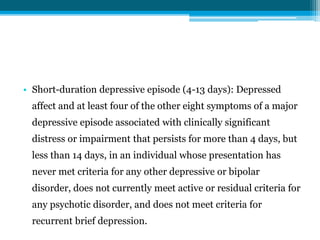
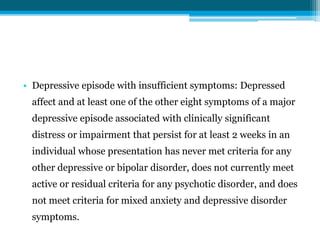
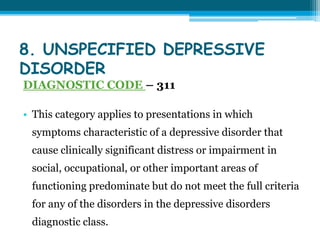
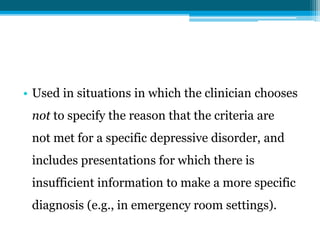
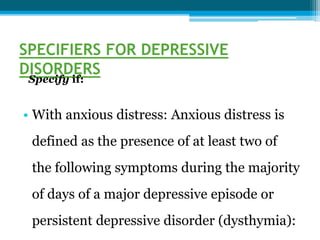
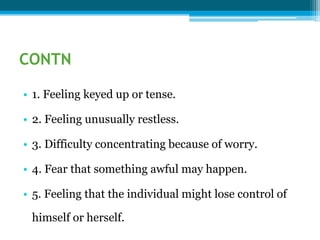
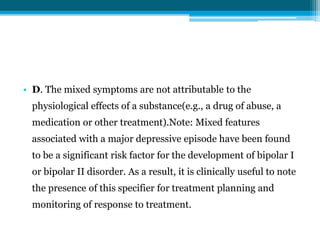
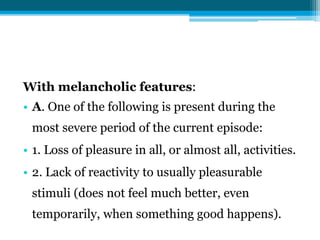
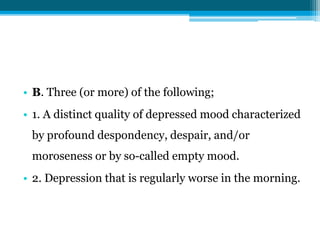
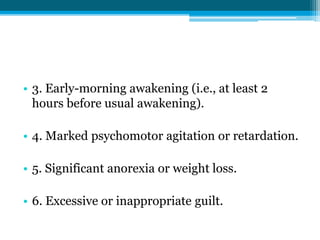
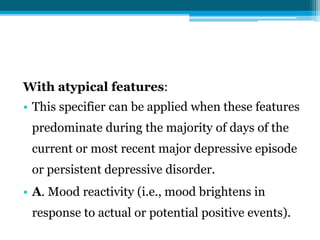
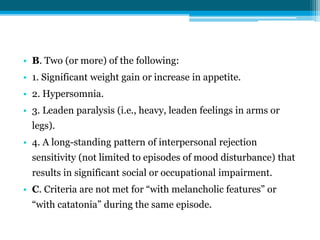
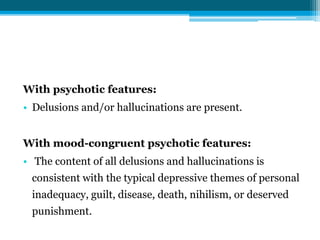
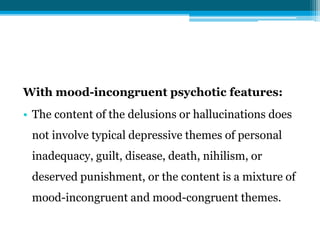
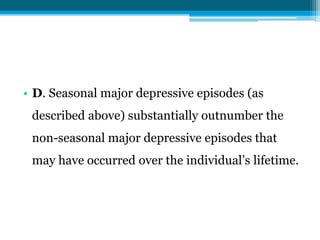
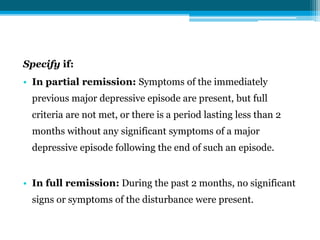
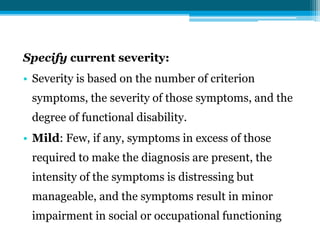
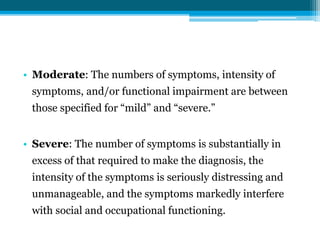
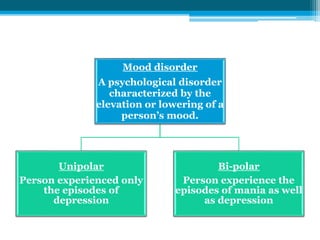
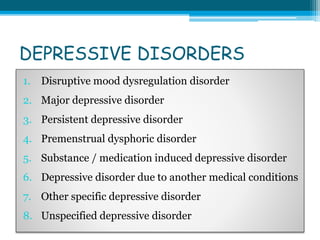
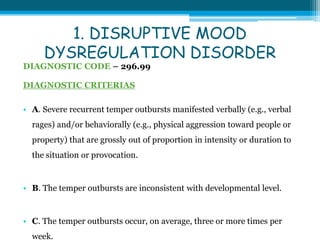
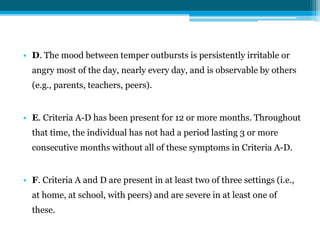
This document provides information on Unipolar Mood Disorder and defines Unipolar Disorder as a mental disorder characterized by pervasive and persistent low mood accompanied by low self-esteem and loss of interest in enjoyable activities. It discusses the manifestations of Unipolar Disorder which can affect daily life for weeks or longer by interfering with social, family, work, academic, and health aspects of life. The document also lists and describes several types of Depressive Disorders including Major Depressive Disorder, Persistent Depressive Disorder, and Premenstrual Dysphoric Disorder. It provides details on the diagnostic criteria, clinical manifestations, causes, assessment tools, prognosis, prevalence, and treatment options for these disorders.
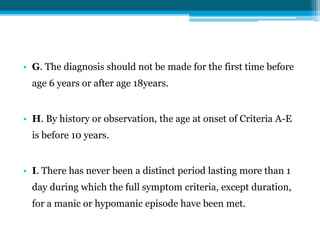
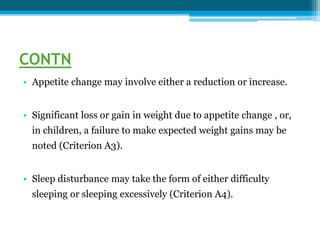
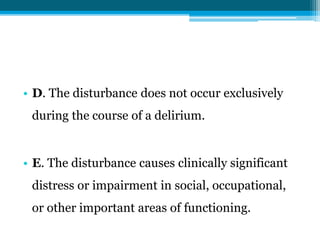
![• J. The behaviors do not occur exclusively during an
episode of major depressive disorder and are not
better explained by another mental disorder (e.g.,
autism spectrum disorder, posttraumatic stress
disorder, separation anxiety disorder, persistent
depressive disorder [dysthymia]).
• K. The symptoms are not attributable to the
physiological effects of a substance or to another
medical or neurological condition.](https://image.slidesharecdn.com/aardra-200125232033/85/UNIPOLAR-MOOD-DISORDER-11-320.jpg)