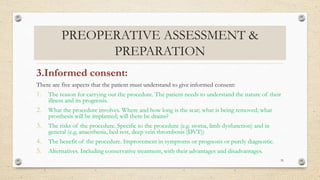
The document discusses the key aspects of preoperative assessment and preparation. It outlines the goals of preoperative assessment as reducing risks, identifying existing medical conditions, and planning management. A thorough assessment involves taking a medical history, physical exam, evaluation of systems like cardiac, respiratory and more. Proper preparation includes discussing the procedure with the patient, obtaining informed consent, giving instructions, and ensuring readiness in the operating theater. The overall aim is to minimize complications and optimize outcomes for the patient's surgery.