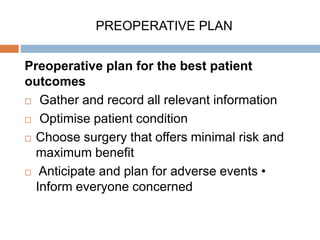
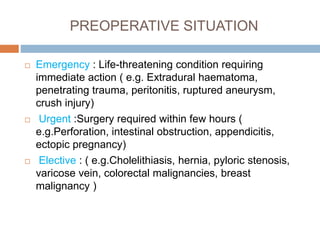
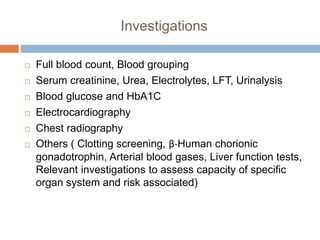
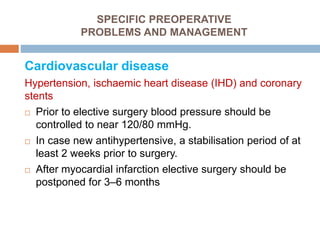
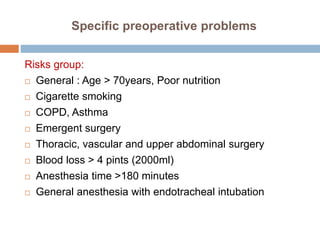
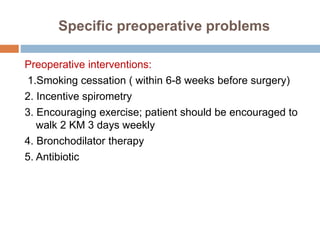
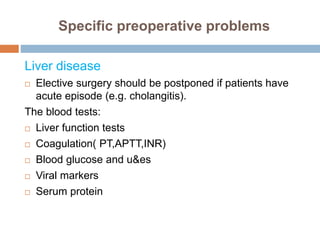
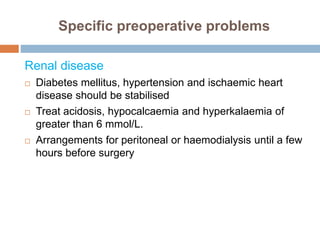
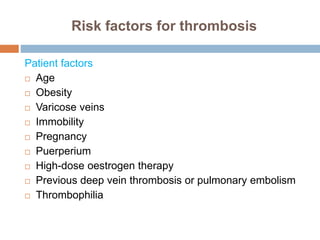
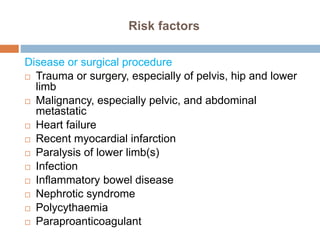
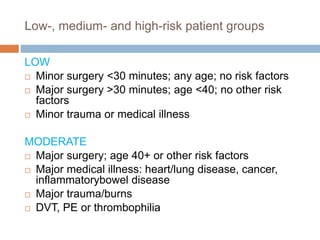
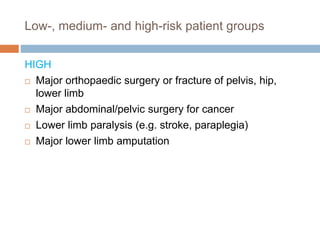
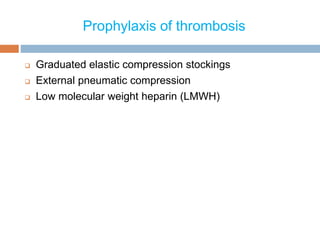
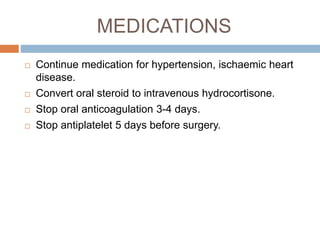
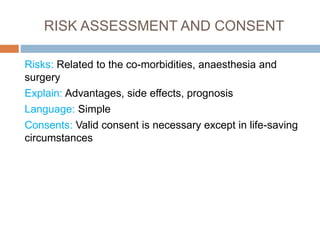
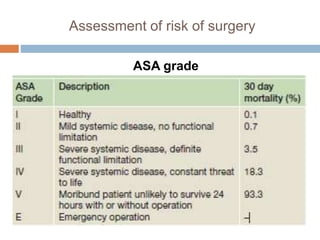
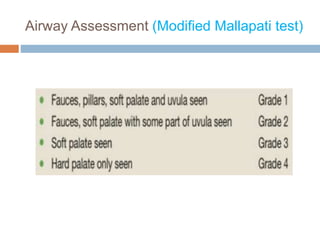
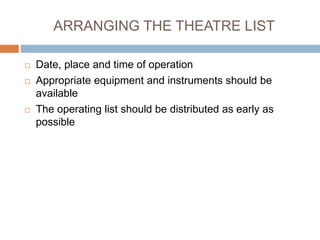
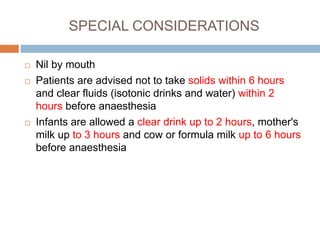
This document discusses preoperative preparation and optimization of surgical patients. It outlines assessing patient history, risk factors, and medical conditions; performing examinations and tests; identifying and managing issues like cardiovascular disease, respiratory disease, diabetes, malnutrition, and coagulation disorders; discussing risks and obtaining consent; and arranging the operating room and prioritizing patients. The goal is to identify and address any factors that could increase surgical risks, and to ensure patients are medically optimized and prepared for their procedures.