This document discusses surgical site infections, including:
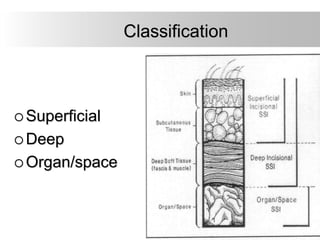
- Surgical site infections are infections that occur within 30 days of a surgical procedure. They are classified as superficial, deep, or organ/space infections.
- Risk factors for surgical site infections include patient factors like diabetes, obesity, and immunosuppression as well as surgical factors like procedure duration and antibiotic prophylaxis.
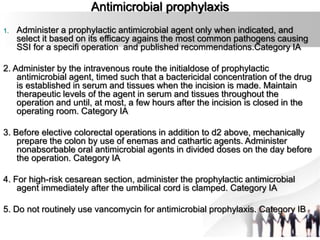
- Proper operating room environment, surgical attire/drapes, aseptic technique and administration of preoperative antibiotics can help prevent surgical site infections. Postoperative incision care and discharge planning are also important.