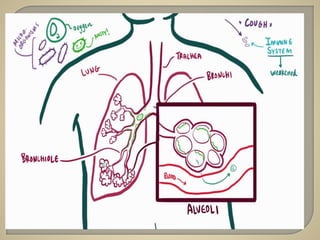
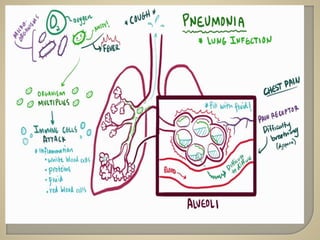
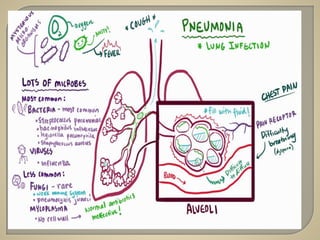
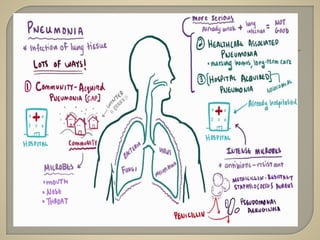
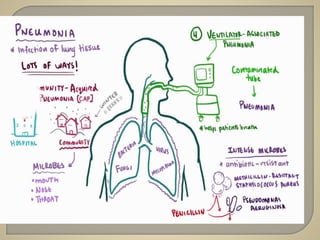
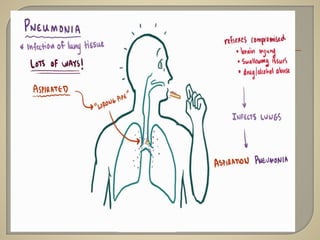
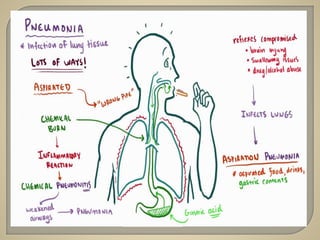
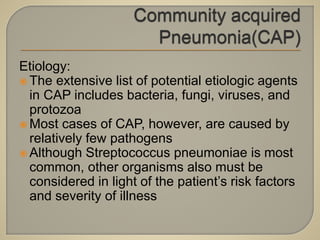
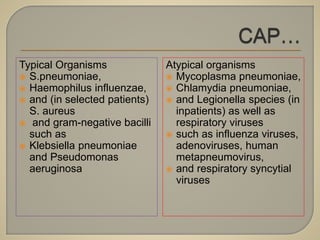
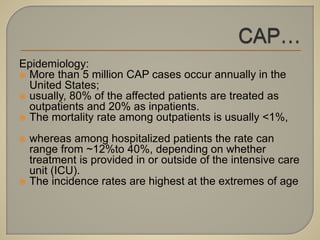
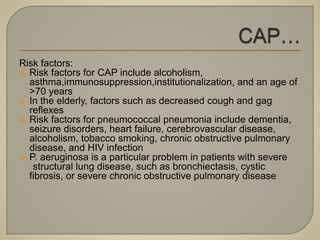
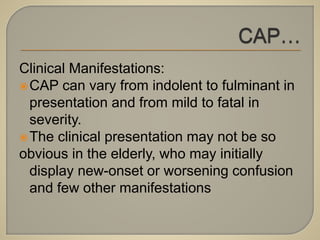
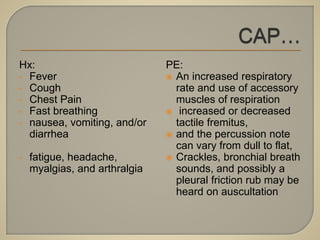
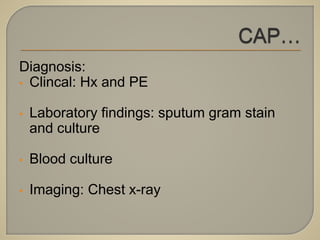
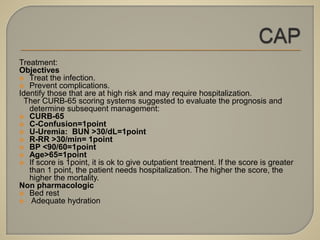
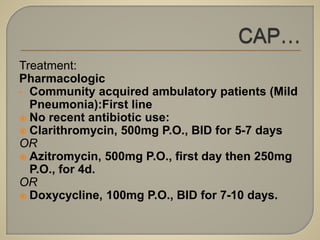
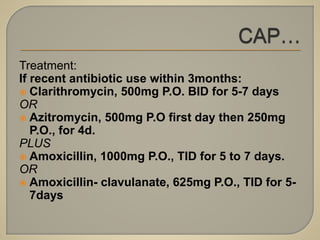
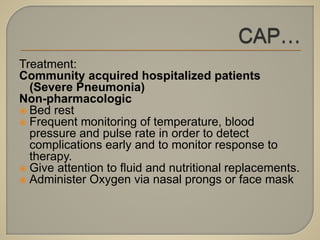
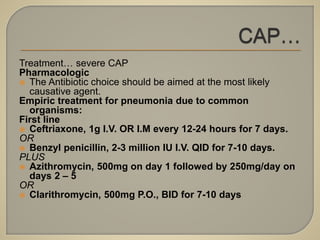
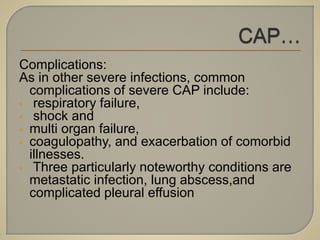
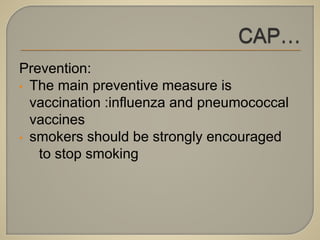
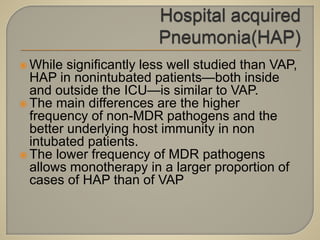
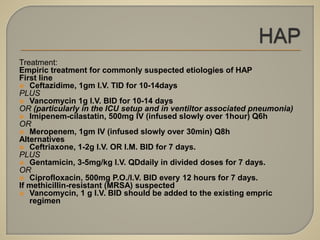
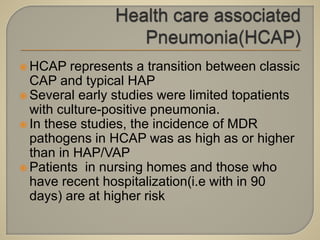
The document provides a comprehensive overview of pneumonia, covering its definition, pathophysiology, etiology, epidemiology, clinical manifestations, diagnosis, treatment, and prevention. It emphasizes the various microbial pathogens responsible for pneumonia, risk factors, and the importance of vaccination and appropriate antibiotic treatment based on patient conditions. The treatment strategies differ significantly between community-acquired and hospital-acquired pneumonia, with special attention to high-risk patients and potential complications.