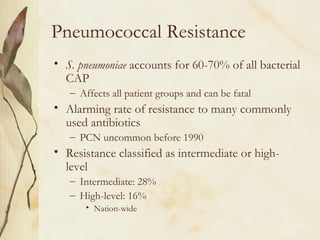
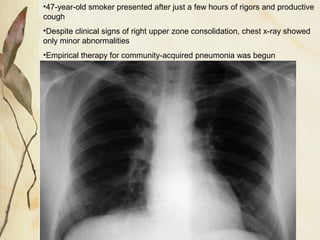
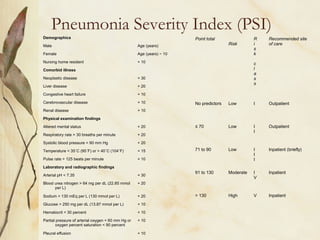
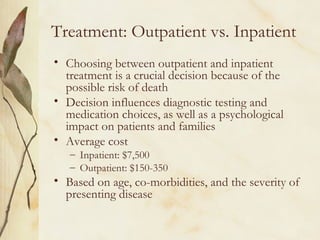
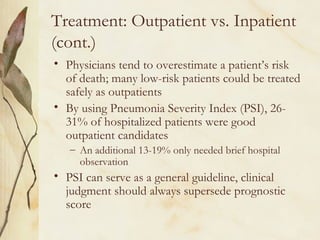
This document provides information on community-acquired pneumonia (CAP). It defines CAP and distinguishes it from other types of pneumonia. It then discusses the epidemiology, clinical presentation, etiology, symptoms, diagnosis, treatment, and antibiotic resistance patterns associated with CAP. Key points include that CAP affects millions annually in the US with high costs, accurate diagnosis and treatment is important to reduce mortality, and resistance to commonly used antibiotics is a concern.



![Pharmacotherapy: Outpatient
• Consensus guidelines
– ATS, Infectious Disease Society of America, and Canadian Guidelines
for the Initial Management of Community-Acquired Pneumonia
• Empiric oral therapy with macrolides, doxycycline, or an
oral beta lactam (amoxicillin, cefuroxime [ceftin], or
amoxicillin/clavulanate [augmentin]), or a
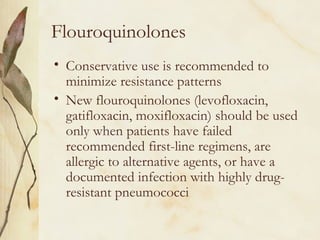
flouroquinolone
– Therapeutic Working Group of the CDC
• Use flouroquinolones sparingly because of resistance concerns
• Duration of therapy
– S. pneumoniae: 7-10 days or until afebrile 3 days
• Bacteremic: 10-14 days
– Mycoplasma/Chlamydia pneumoniae: 10-14 days, up to 21 days
– Legionella: 10-21 days](https://image.slidesharecdn.com/communityacquiredpneumoniacap-140529071542-phpapp01/85/Community-acquired-pneumonia-cap-20-320.jpg)
![Pharmacotherapy: Outpatient
(cont.)
• Several classes of antibiotics are effective against atypical
pathogens
• C. pneumoniae and Legionella species are intracellular
organisms and M. pneumoniae lacks a cell wall, beta
lactams are not effective
– Erythromycin and tetracycline have been traditional choices for
atypical CAP
– Newer macrolides (azithromycin [zithromax] and
clarithromycin [biaxin]) have good atypical activity and are
generally are better tolerated than erythromycin
– Doxycycline (Vibramcyin) is effective, associated with fewer
gastrointestinal side effects, and is a less expensive alternative
– Flouroquinolones have demonstrated excellent activity against
atypicals and have one-daily dosing and excellent bioavailability](https://image.slidesharecdn.com/communityacquiredpneumoniacap-140529071542-phpapp01/85/Community-acquired-pneumonia-cap-21-320.jpg)
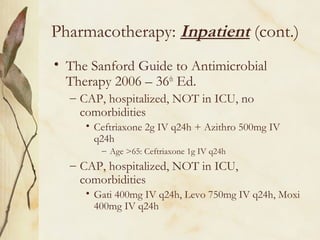
![Pharmacotherapy: Inpatient
• Antibiotic therapy should be initiated within 4
hours of hospitalization
• Intravenous beta lactam (cefotaxime [claforan]
or ceftriaxone [rocephin]) plus a macrolide or a
combination of ampicillin/sulbactam (unasyn)
plus a macrolide or a fluoroquinolone alone
• After clinically stable (T<100.0, HR<100,
RR<24, SBP>90, O2 sat>90%) and able to
tolerate oral intake, may be switched to oral
antibiotics for remainder of therapy
– Save money, earlier discharge, minimizes risk of
nosocomial infections](https://image.slidesharecdn.com/communityacquiredpneumoniacap-140529071542-phpapp01/85/Community-acquired-pneumonia-cap-24-320.jpg)