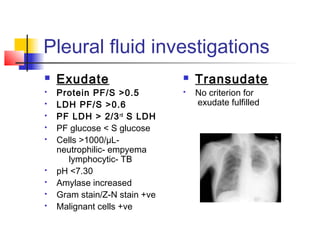
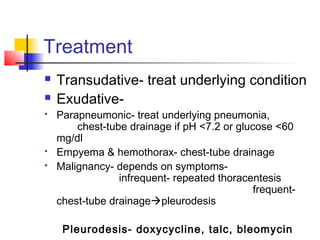
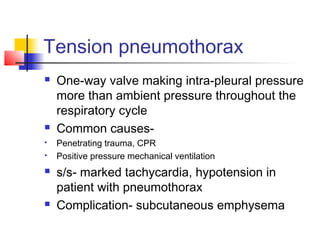
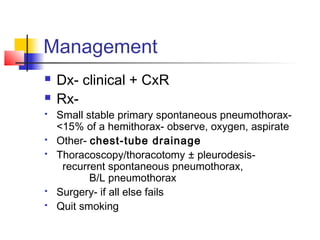
Pleural diseases include pleural effusions, pneumothorax, and mesothelioma. Pleural effusions are abnormal fluid accumulations in the pleural space that can result from increased fluid production, decreased lymphatic drainage, infection, or bleeding. Evaluation involves symptoms, chest x-ray, ultrasound, and thoracentesis. Treatment depends on whether the effusion is transudative or exudative. Pneumothorax is the presence of air in the pleural space and can be caused by trauma, lung blebs, or underlying lung disease. Tension pneumothorax is life-threatening due to increased intra-pleural pressure. Management involves chest tube drainage or surgery depending on the situation