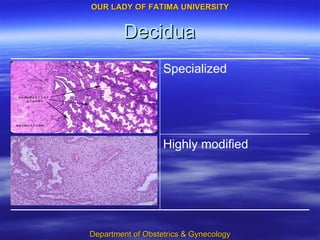
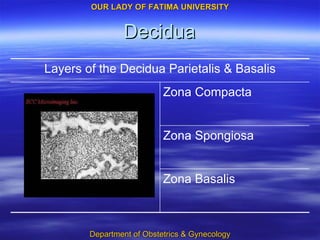
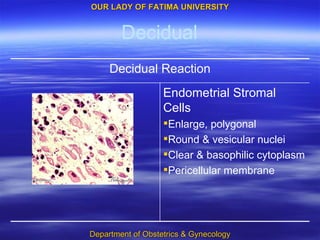
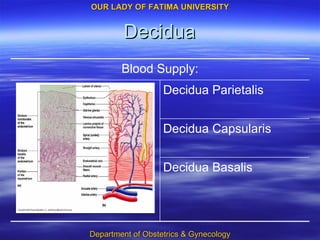
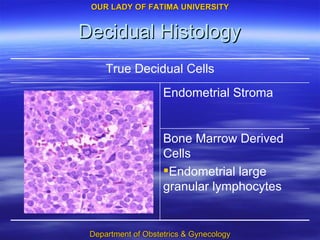
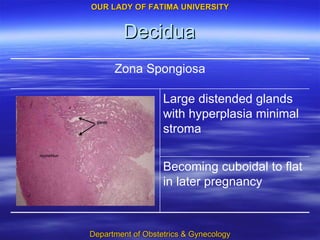
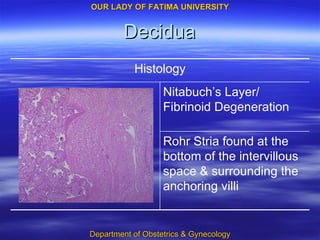
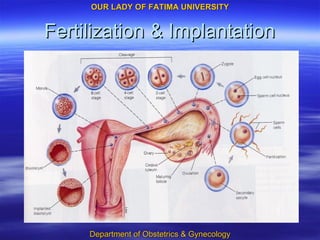
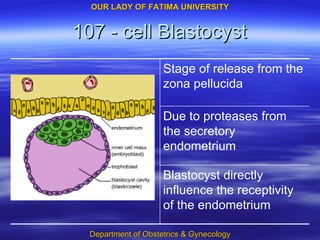
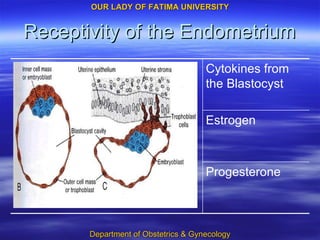
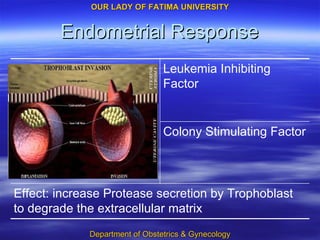
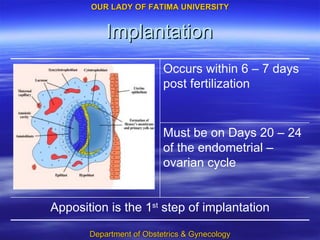
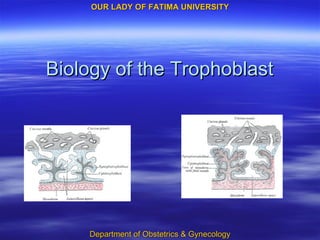
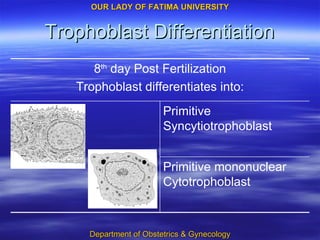
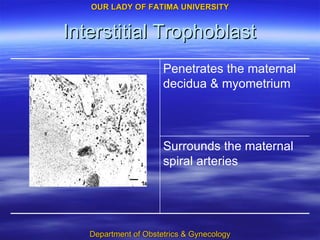
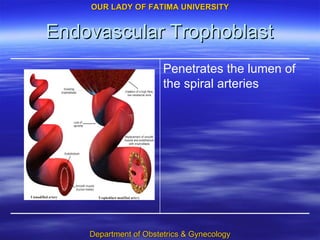
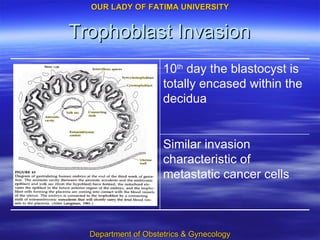
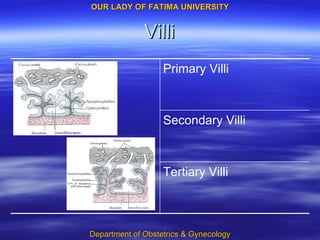
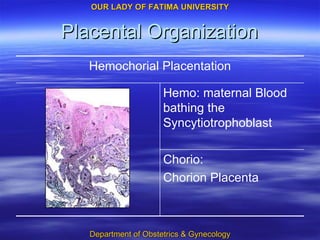
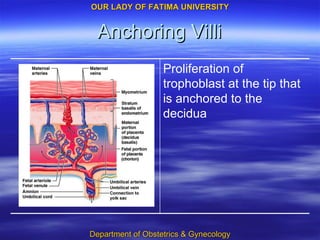
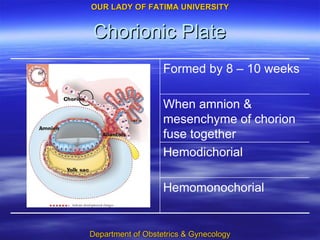
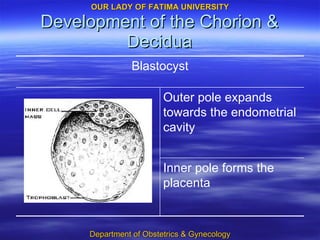
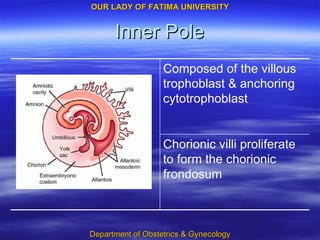
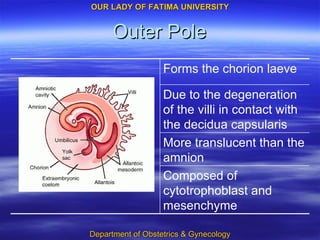
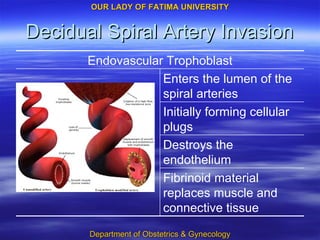
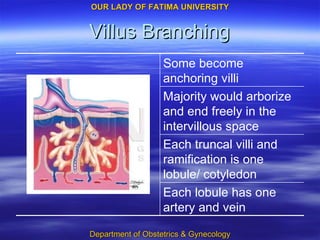
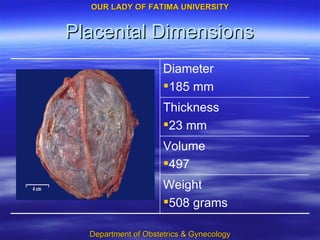
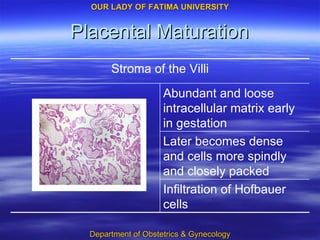
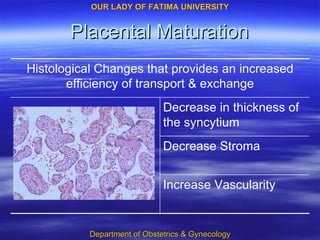
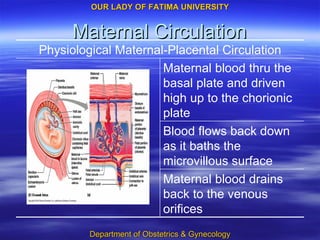
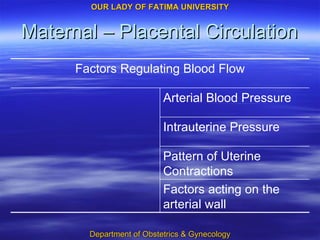
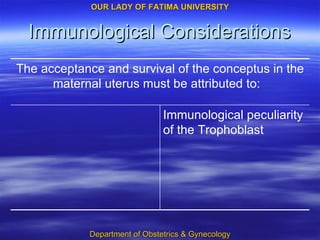
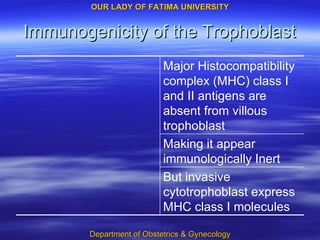
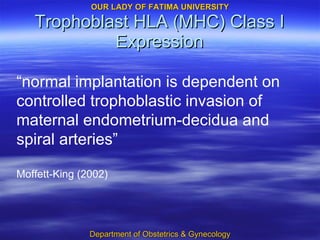
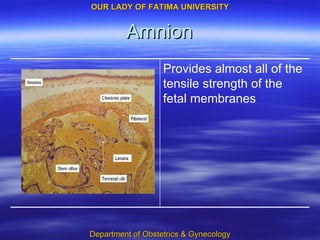
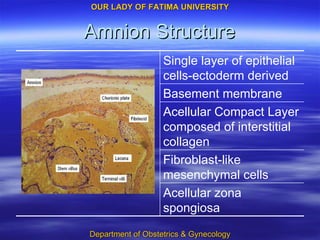
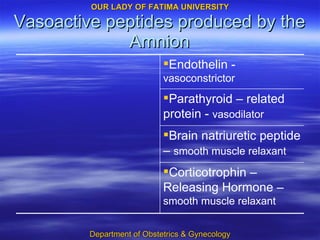
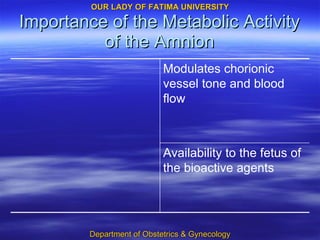
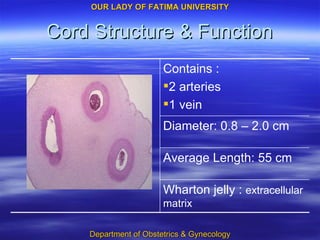
The document discusses the placenta, fetal membranes, decidua, trophoblast, and amnion. It describes their structure, development, functions, and roles in implantation, fetal-maternal circulation and immunological acceptance of pregnancy. Key points include how the decidua and trophoblast interact for implantation, trophoblast invasion of maternal spiral arteries, establishment of maternal blood flow, and the metabolic and protective roles of the amnion and fetal membranes.