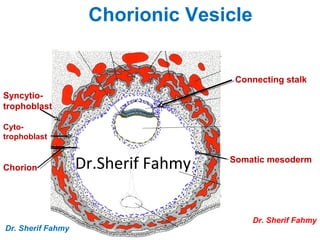
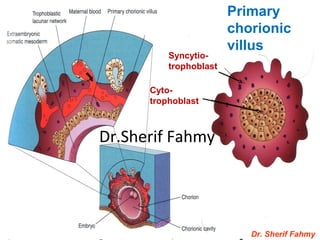
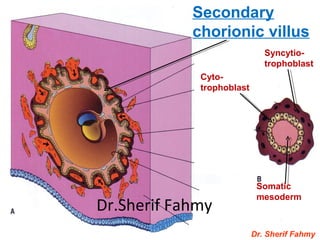
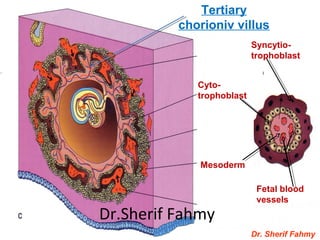
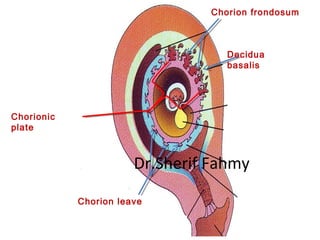
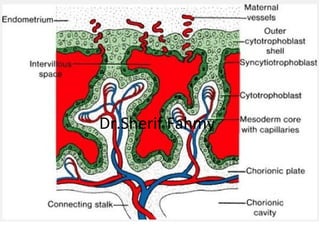
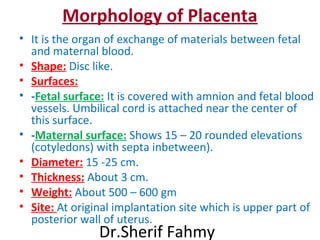
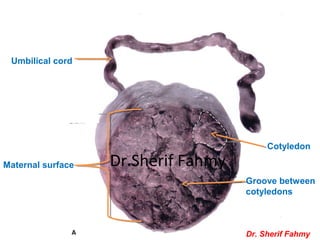
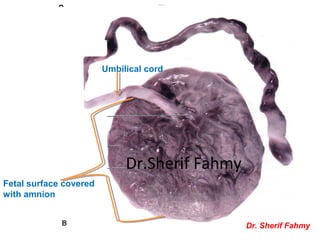
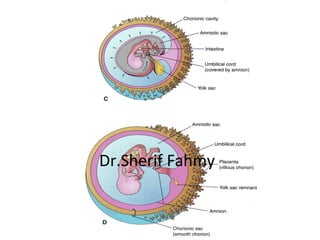
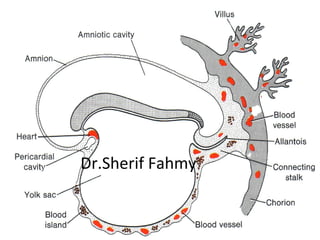
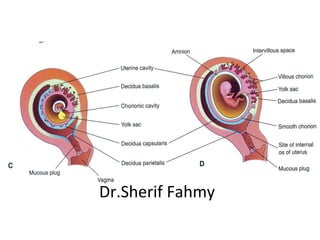
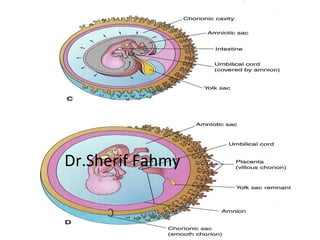
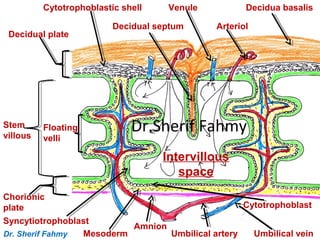
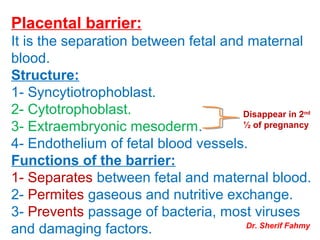
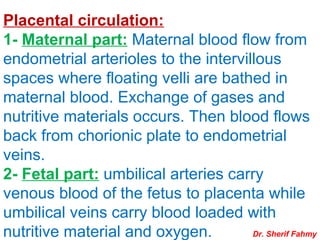
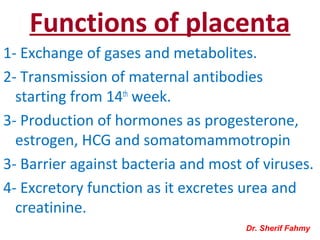
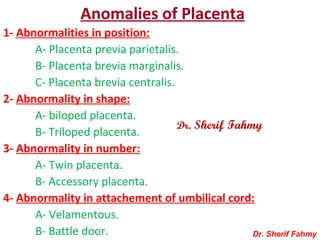
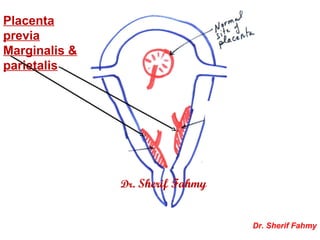
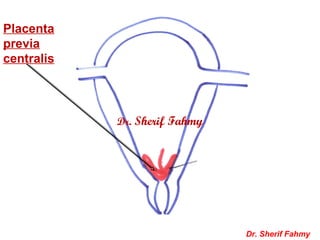
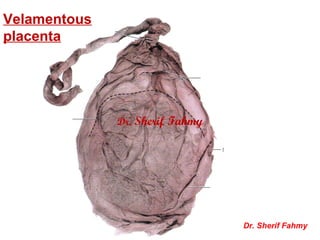
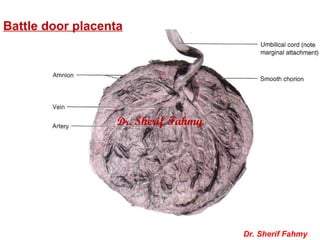
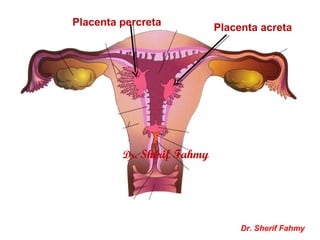
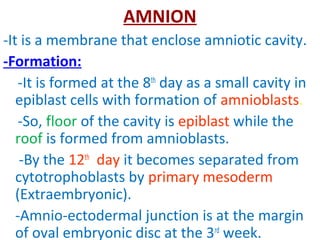
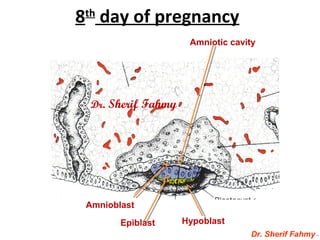
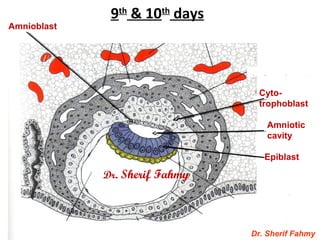
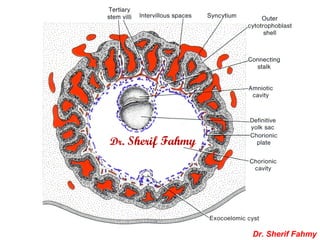
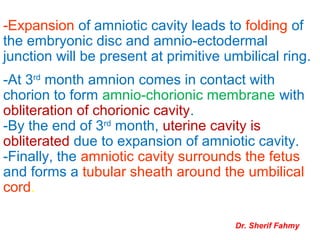
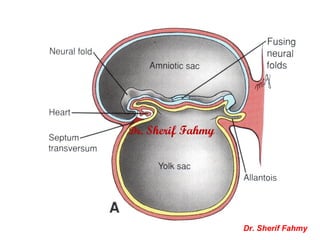
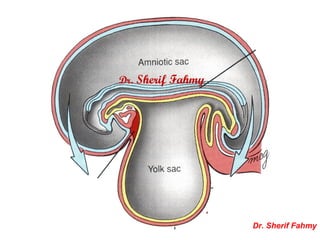
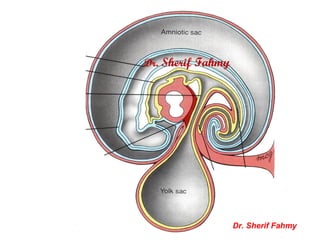
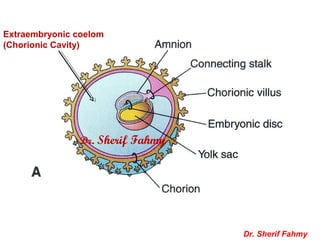
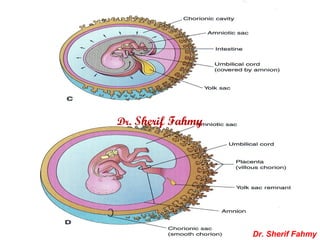
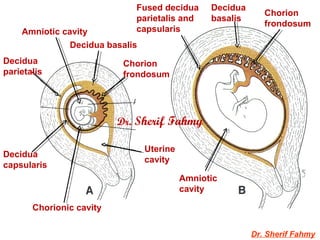
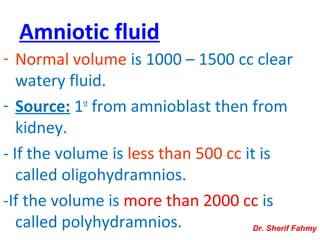
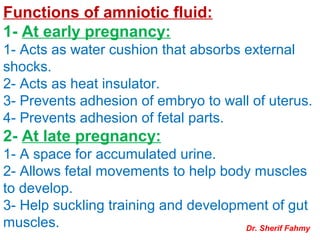
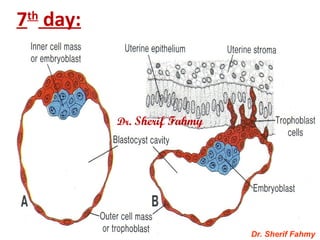
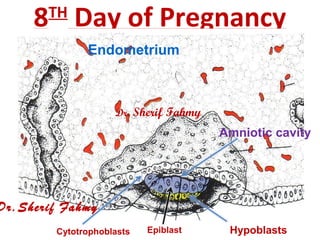
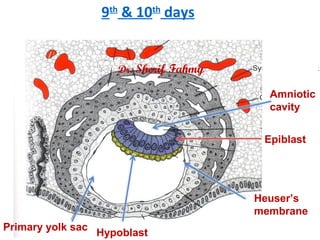
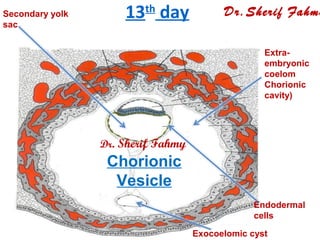
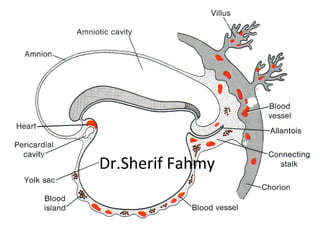
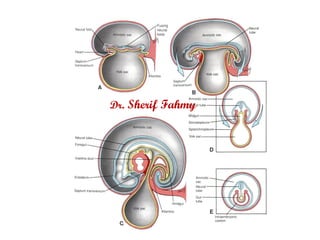
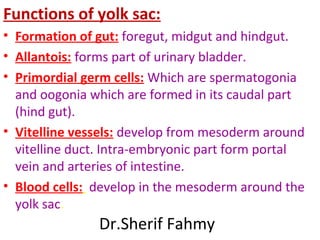
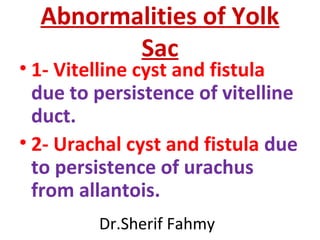
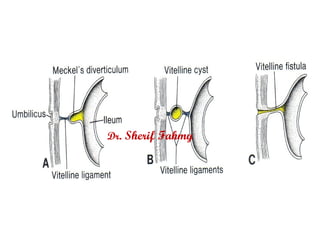
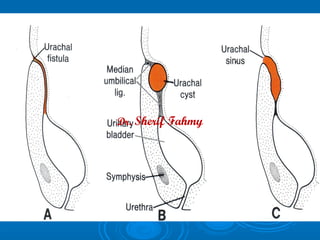
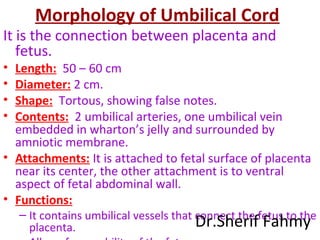
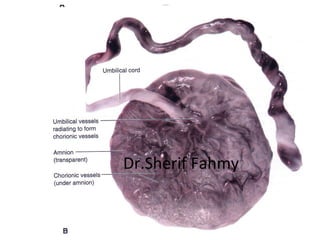
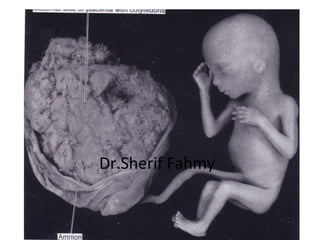
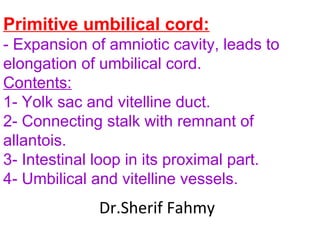
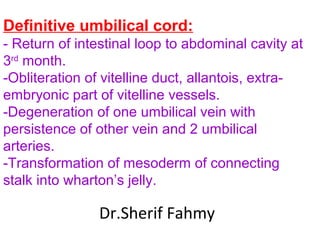
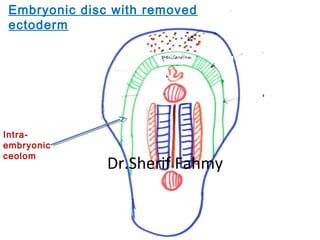
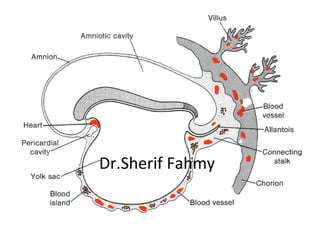
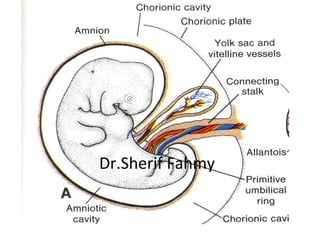
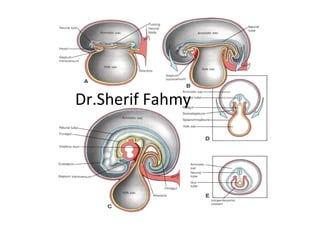
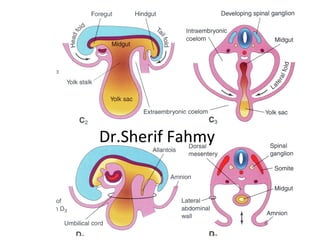
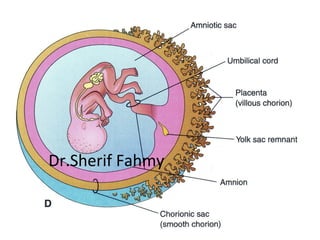
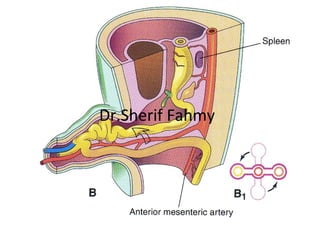
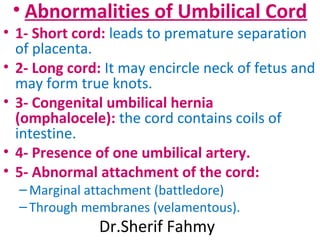
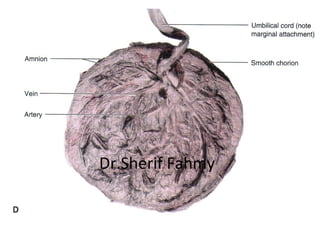
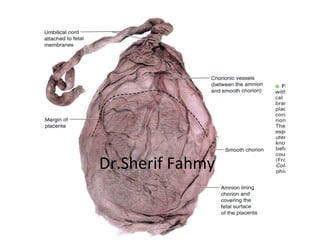
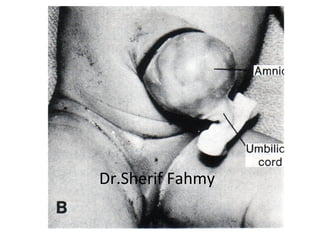
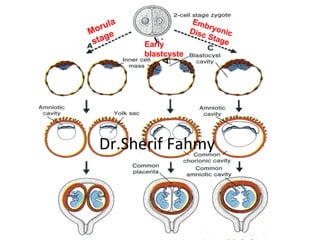
The document discusses the fetal membranes including the chorion, placenta, amnion, and umbilical cord. It describes their formation, structure, development, functions, and some abnormalities. The chorion forms early in development and differentiates into chorionic villi. The placenta develops from the chorion and facilitates gas/nutrient exchange between mother and fetus. The amnion forms a sac surrounding the fetus filled with amniotic fluid. The umbilical cord contains blood vessels connecting the fetus to the placenta.