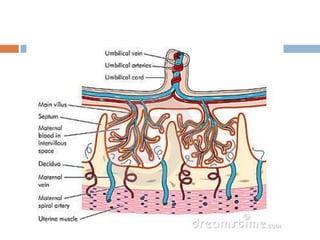
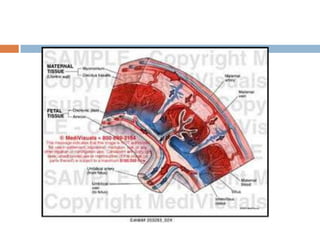
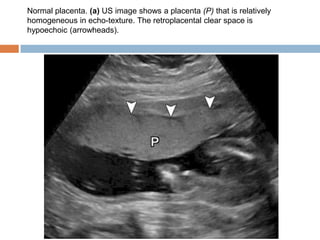
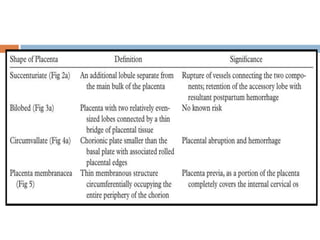
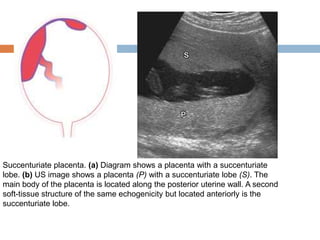
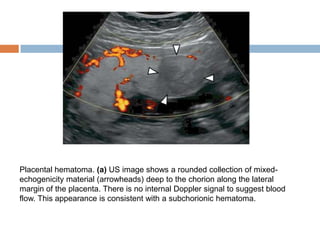
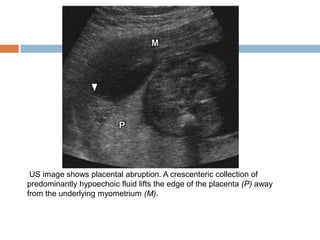
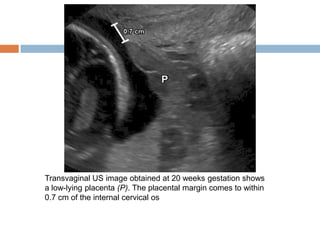
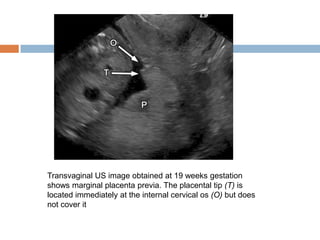
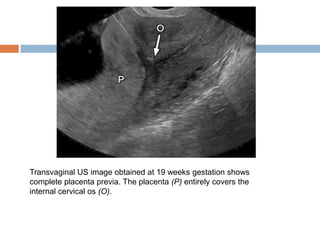
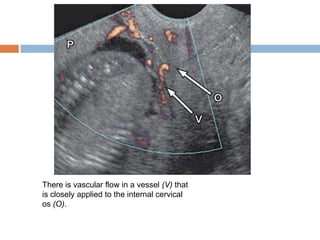
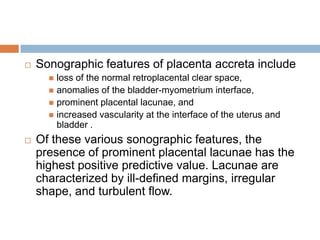
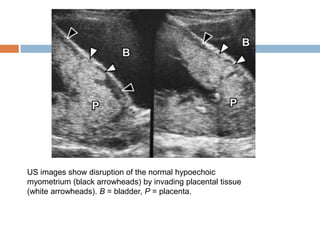
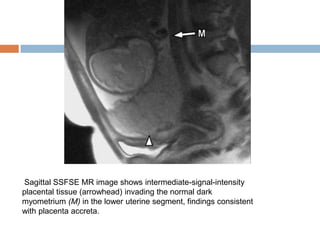
This document discusses imaging of the placenta. Sonography is the preferred imaging modality for evaluating the placenta due to its ability to characterize tissue without radiation exposure. Magnetic resonance imaging can provide additional information, particularly for invasive placental processes like placenta accreta. Computed tomography has a limited role due to poorer tissue characterization and radiation risk to the fetus. The document describes normal placental anatomy and variants, as well as placental pathologies that can cause antepartum hemorrhage like placenta previa, placental abruption, and placental hematomas.