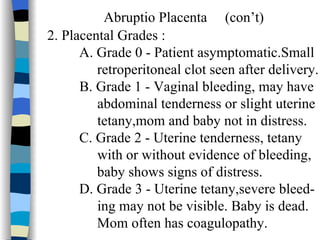
The document discusses several types of placental abnormalities including abruptio placenta, placenta previa, placenta accreta, and other rare conditions. Abruptio placenta is the premature separation of the placenta from the uterus after 20 weeks of gestation. Placenta previa occurs when the placenta implants in the lower uterine segment, covering all or part of the cervical os. Placenta accreta involves abnormal placental attachment to the myometrium, which can cause life-threatening bleeding during delivery.