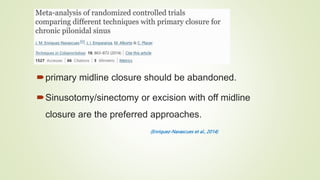
Pilonidal sinus disease is a common condition affecting young adults. Treatment options range from minimally invasive to surgical excision. Guidelines recommend excision with off-midline closure techniques like Limberg flap or Karydakis procedure to minimize recurrence rates. Surgical treatment should be individualized based on patient and surgeon preference. Minimally invasive techniques may be suitable for small primary disease but flap reconstruction is preferred for complex recurrent cases.