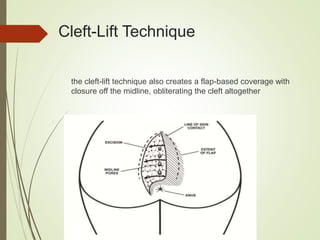
This document provides an overview of pilonidal disease management. It discusses the epidemiology, etiology, risk factors, evaluation, and various treatment approaches for both acute and chronic pilonidal disease. For acute disease, incision and drainage is the mainstay of treatment. For chronic disease, options include excision with primary closure, healing by secondary intention, marsupialization, or flap procedures. The document recommends uniform guidelines to reduce recurrence rates and time to return to work.









![References
Iesalnieks I, Ommer A, Petersen S, Doll D, Herold A. German national guideline on the
management of pilonidal disease. Langenbecks Arch Surg. 2016;401:599–609. [PubMed]
M Chance Spalding(2018, January 26). Pilonidal Disease Guidelines. Retrieved March 12, 2018,
from https://emedicine.medscape.com/article/192668-guidelines
Matter, I., Kunin, J., Schein, M. and Eldar, S. (1995), Total excision versus non-resectional
methods in the treatment of acute and chronic pilonidal disease. Br J Surg, 82: 752–753.
doi:10.1002/bjs.1800820612
Saber, A. (2014). Modified Off-Midline Closure of Pilonidal Sinus Disease. North American
Journal of Medical Sciences, 6(5), 210–214. http://doi.org/10.4103/1947-2714.132936
Smart, P. J., Dungerwalla, M. & Heriot, A. G. Bascom’s Simple Pilonidal Sinus Surgery: Simpler
with Ultrasound Guidance.Journal of Medical Ultrasound 21, 97–
99,https://doi.org/10.1016/j.jmu.2013.04.001 (2013).
Steele SR, Perry WB, Mills S, Buie WD, Standards Practice Task Force of the American Society
of Colon and Rectal Surgeons. Practice parameters for the management of pilonidal disease. Dis
Colon Rectum. 2013 Sep. 56 (9):1021-7
Yoldas, T., Karaca, C., Unalp, O., Uguz, A., Caliskan, C., Akgun, E., & Korkut, M. (2013).
Recurrent Pilonidal Sinus: Lay Open or Flap Closure, Does It Differ?International Surgery, 98(4),
319–323. http://doi.org/10.9738/INTSURG-D-13-00081.1
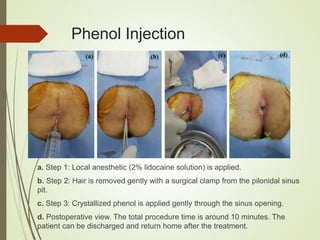
Yuksel, M. E. (2016). Pilonidal sinus disease can be treated with crystallized phenol using a
simple three-step technique. Acta Dermatovenerologica Alpina Pannonica et Adriatica, 26(1).
doi:10.15570/actaapa.2017.4](https://image.slidesharecdn.com/pilonidaldiseaseguidliness-180526225653/85/Pilonidal-Disease-Management-Approach-30-320.jpg)
