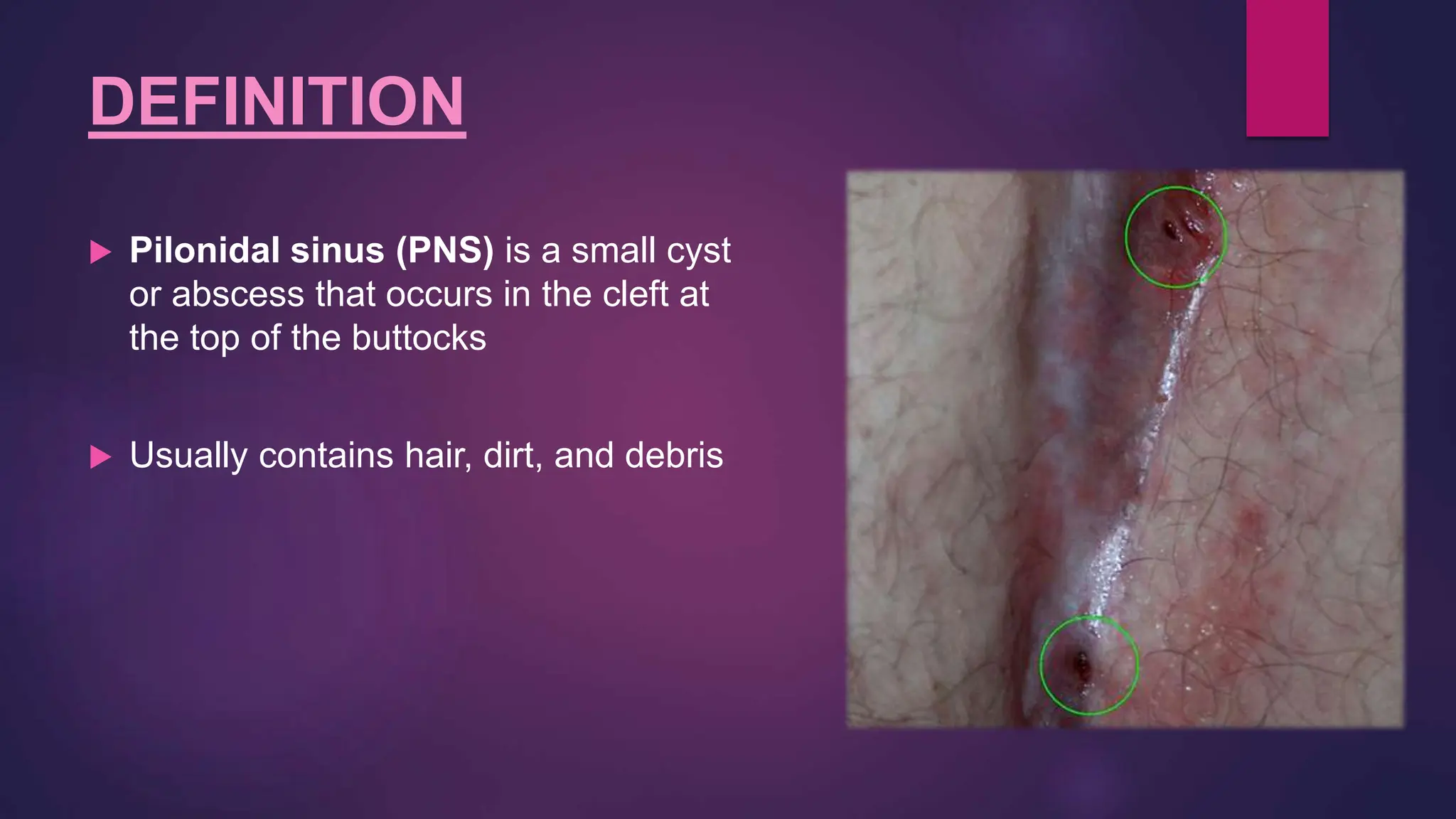
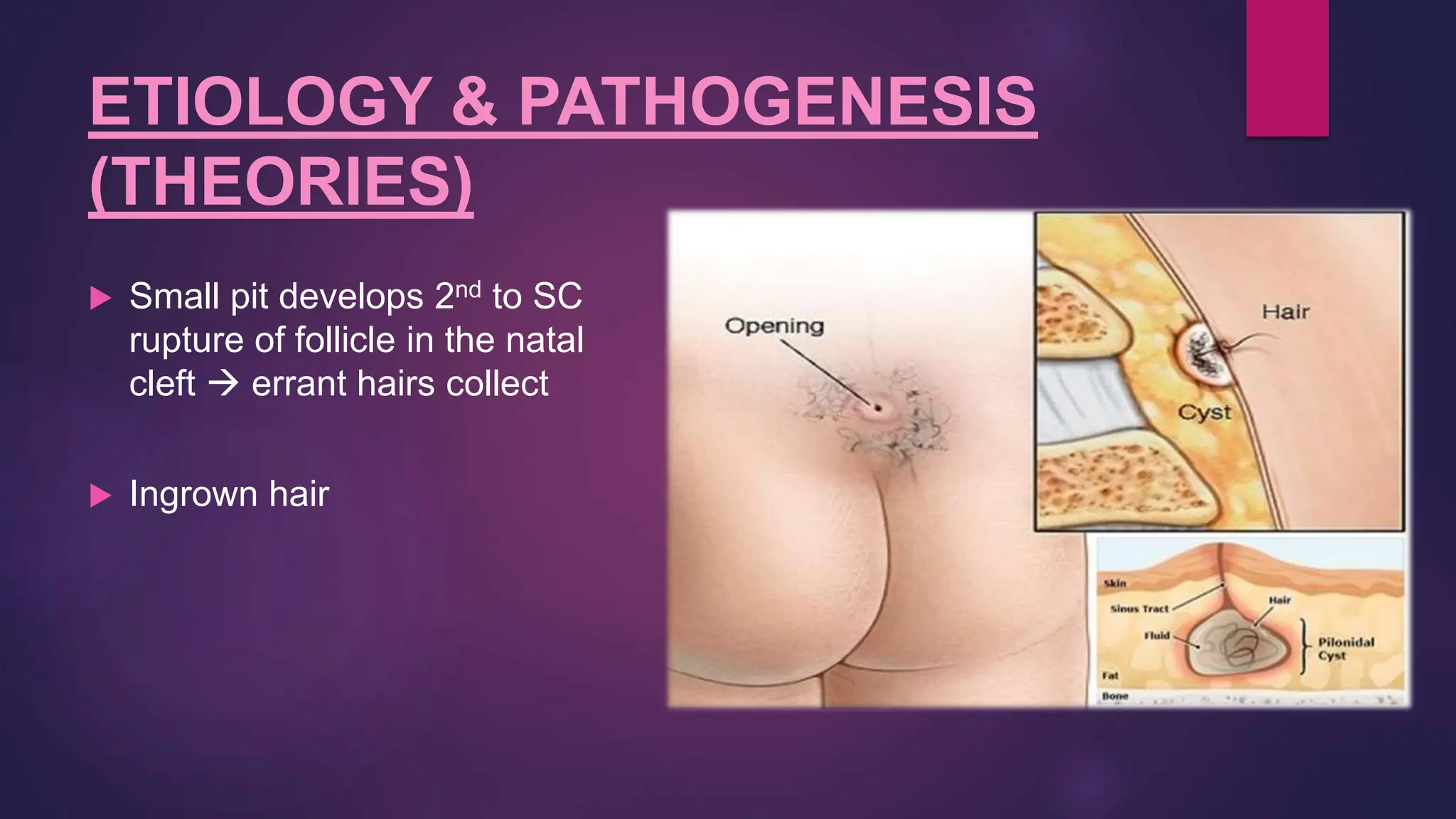
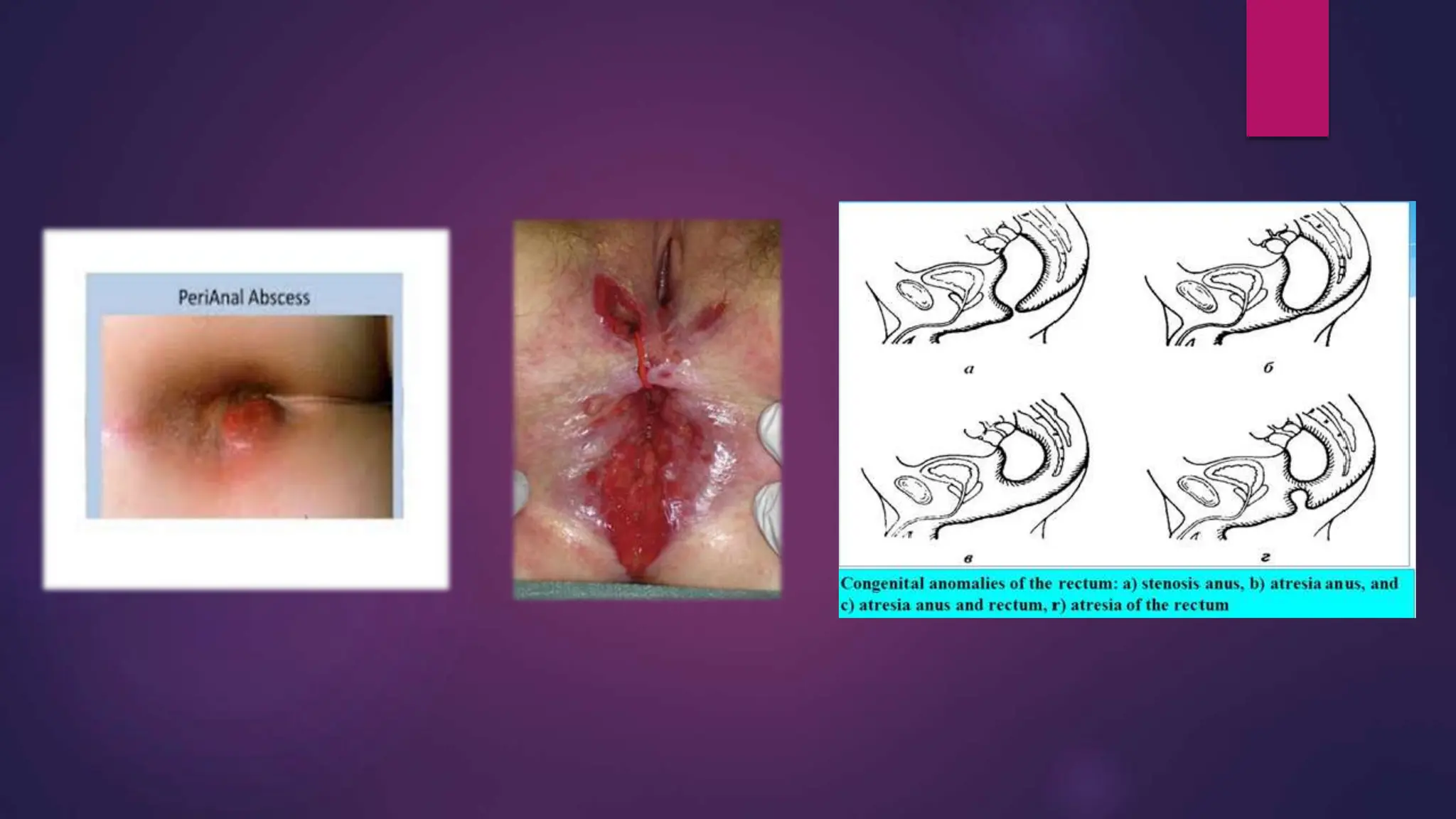
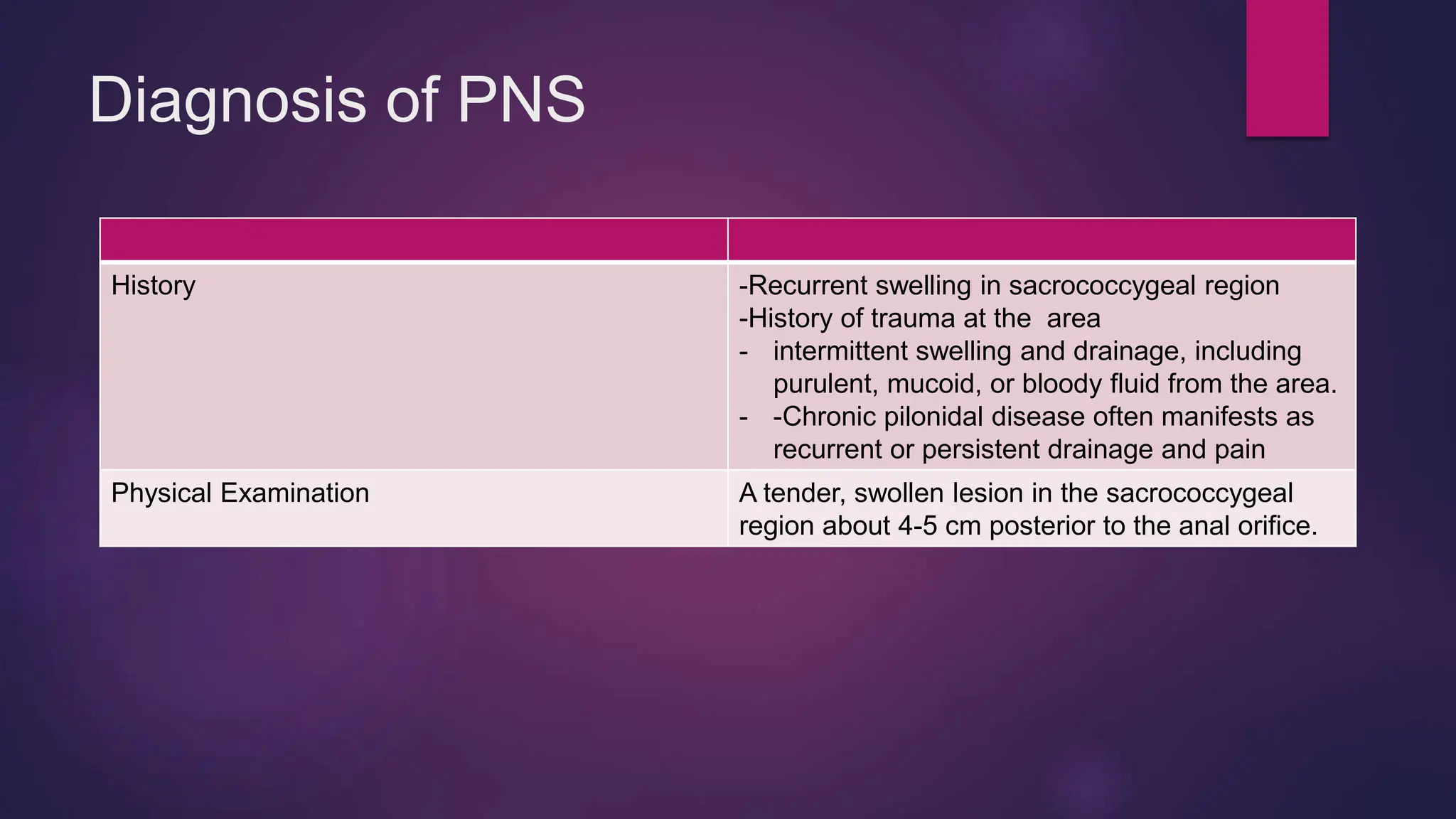
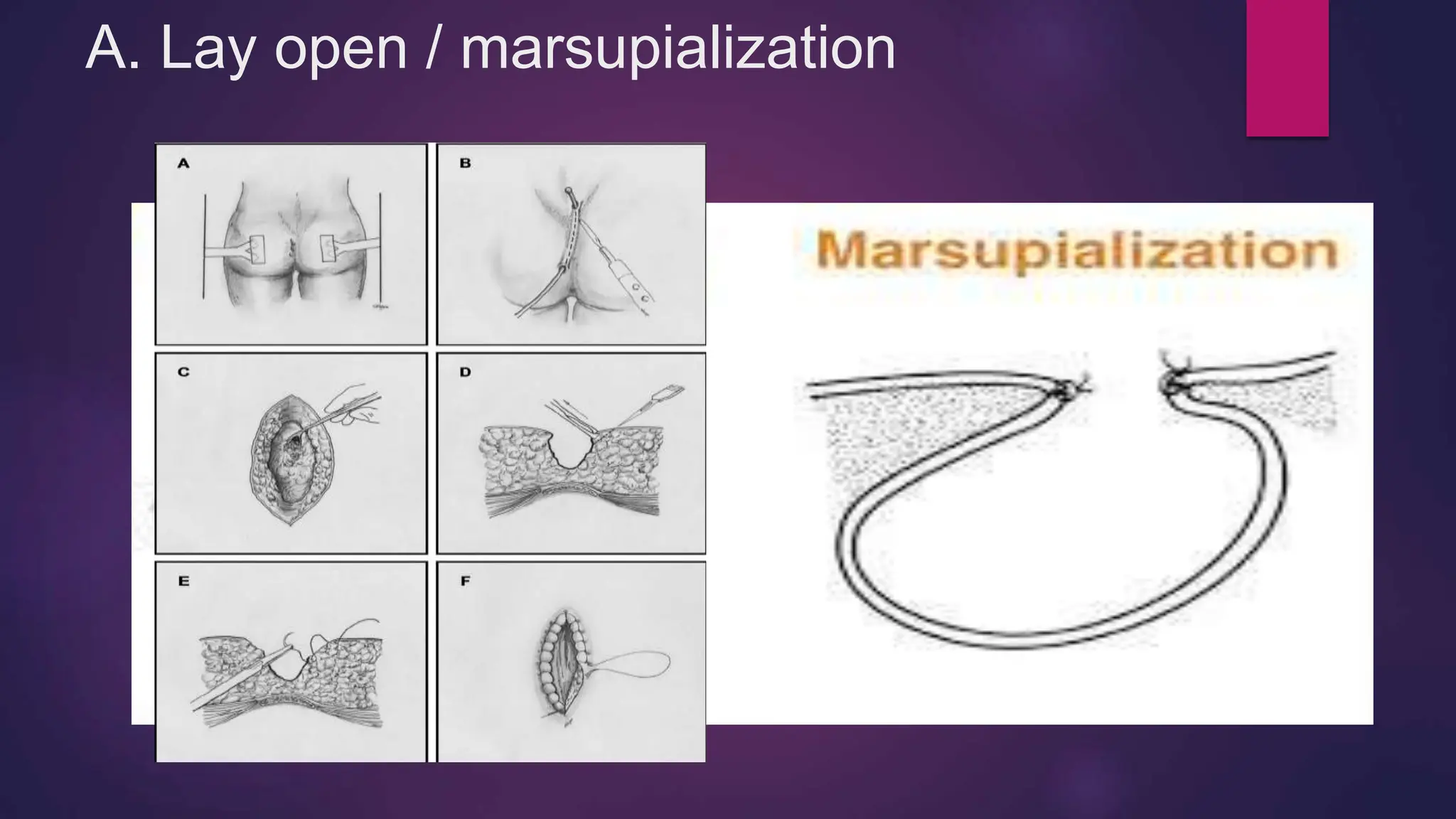
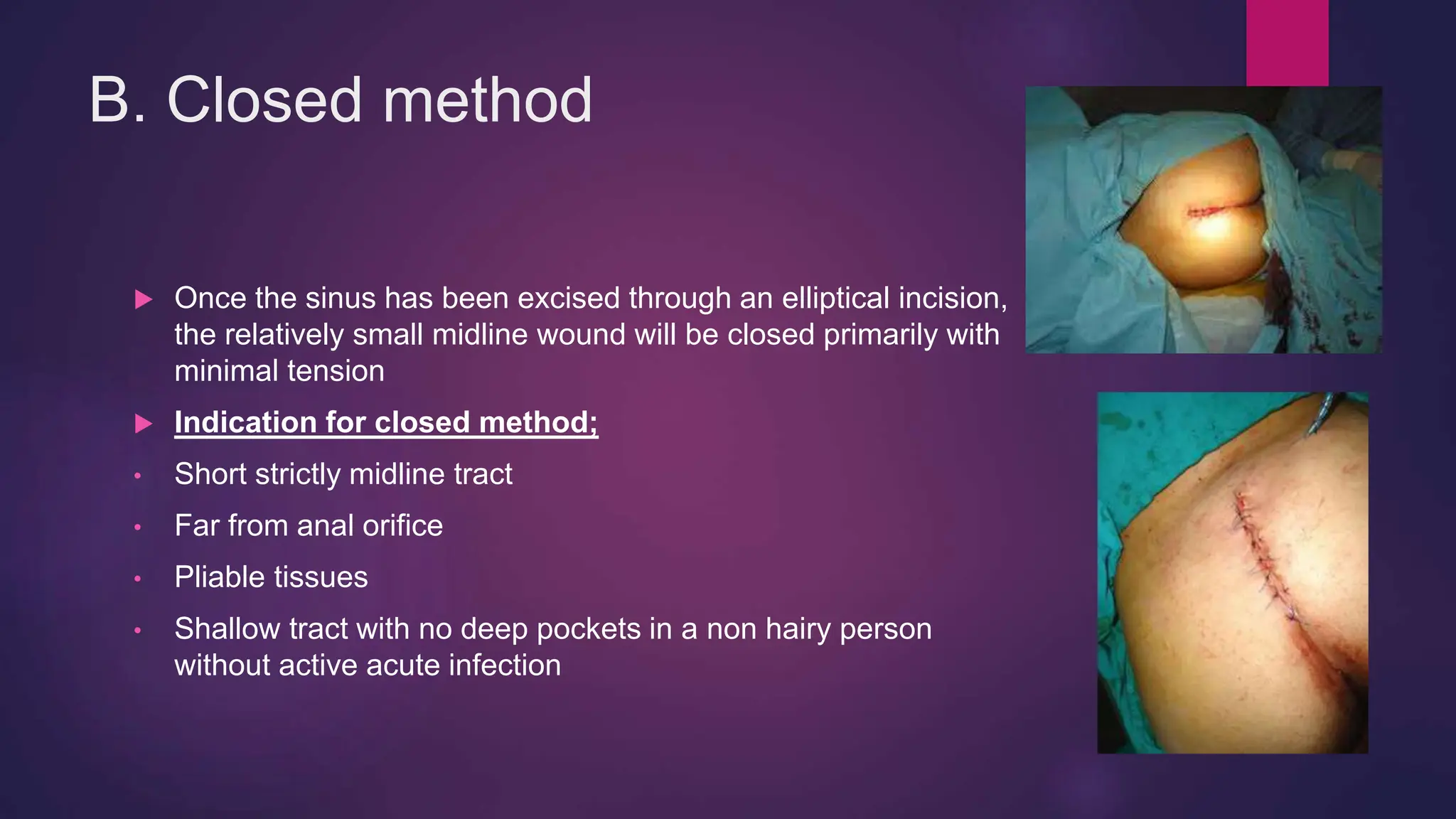
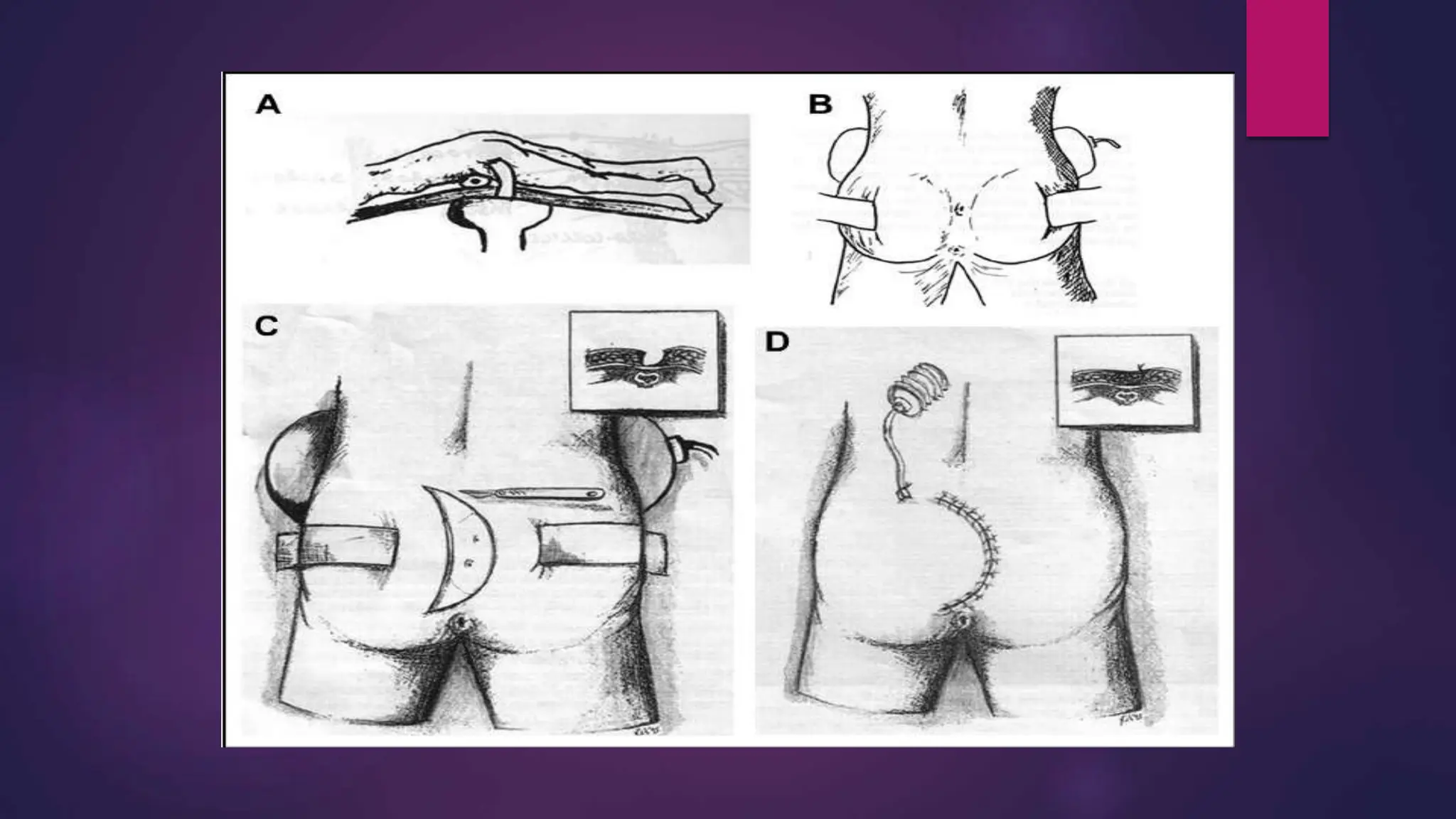
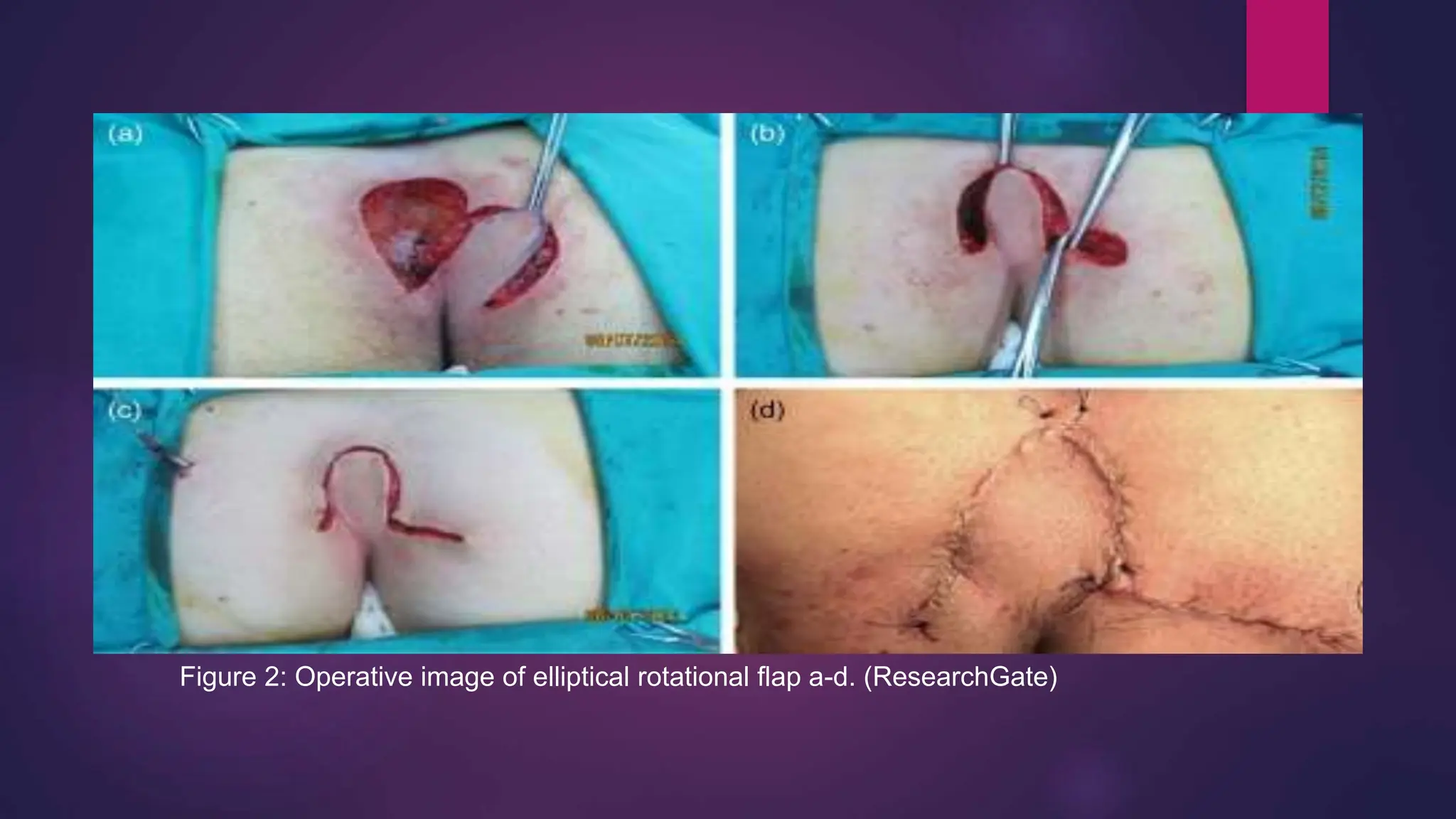
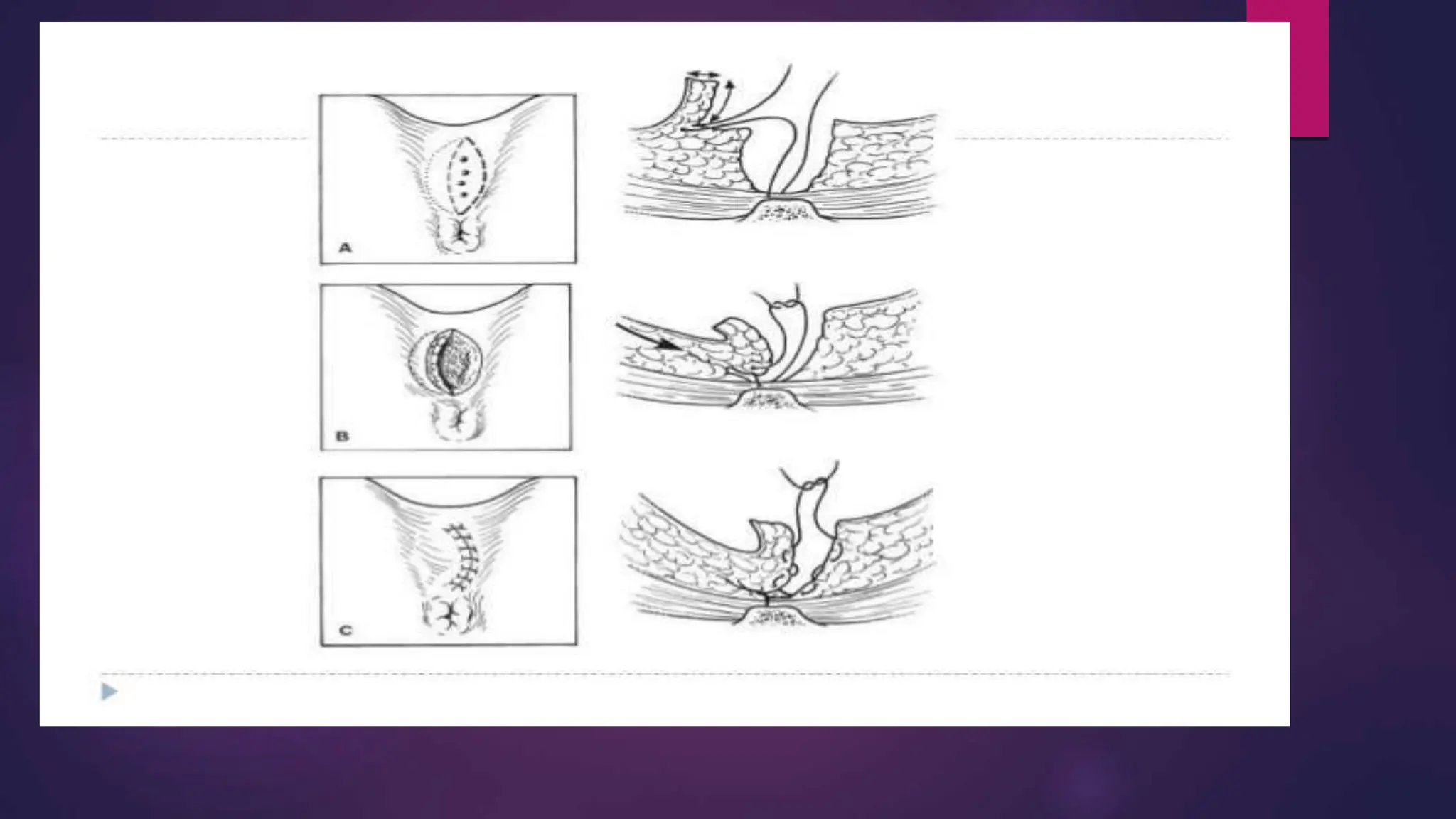
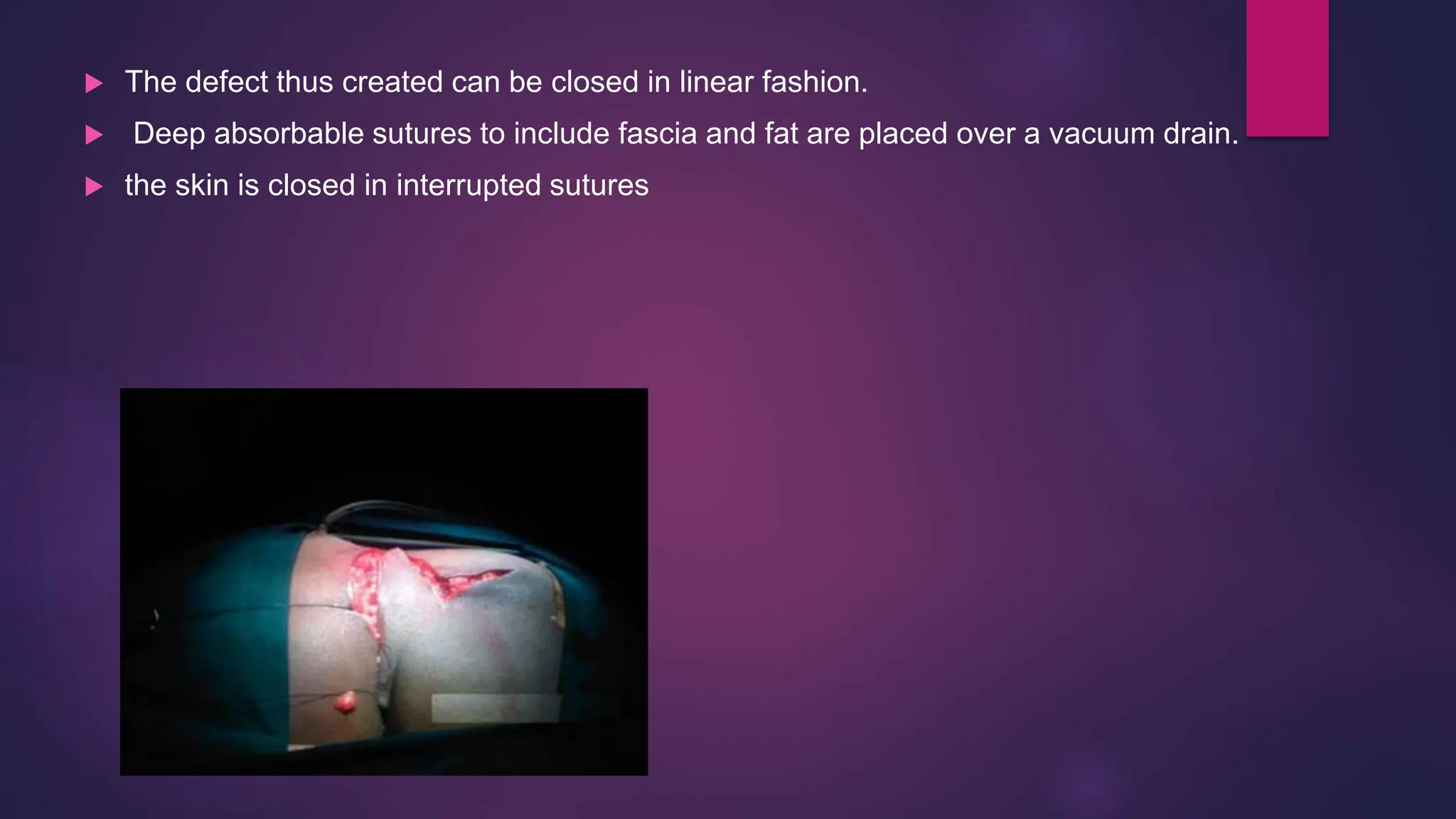
This document discusses pilonidal sinus, which is a cyst or abscess that occurs in the cleft of the buttocks, usually containing hair, dirt or debris. It presents a risk for males with hirsutism who spend long periods sitting. Clinically it presents as an acute abscess or chronic recurring pain. Differential diagnoses include anal fistulas or hidradenitis suppurativa. Treatment involves incision and drainage for abscesses or sinus excision and closure. Recurrent or complex cases may require Z-plasty, V-Y flaps or rotational flaps. Complications can include recurrence, bleeding or infection. Prognosis depends on severity but most cases heal well with 4 weeks for s