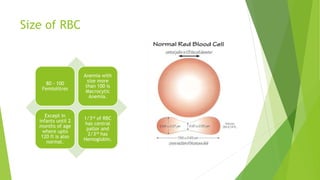
1) Macrocytic anemia is characterized by abnormally large red blood cells (RBCs) over 100 femtoliters in size. It can be classified as megaloblastic or non-megaloblastic.
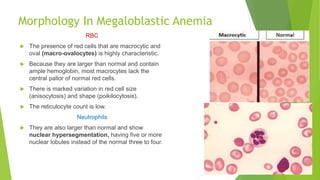
2) Megaloblastic anemia is caused by a failure of DNA synthesis that results in ineffective hematopoiesis and abnormally large and misshapen RBCs and neutrophils. It includes pernicious anemia and deficiencies in vitamin B12 and folate.
3) Pernicious anemia is an autoimmune disorder caused by lack of intrinsic factor needed for vitamin B12 absorption in the stomach, most commonly affecting older adults.