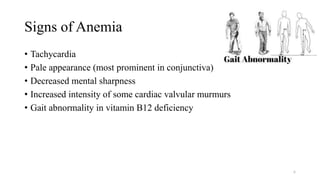
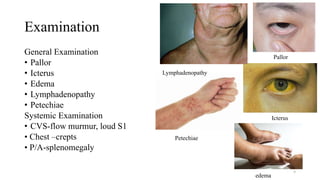
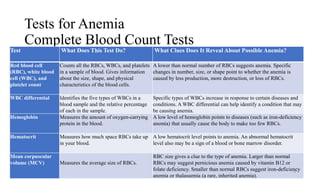
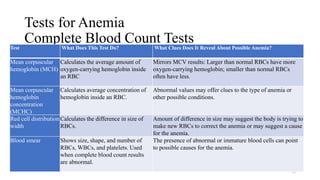
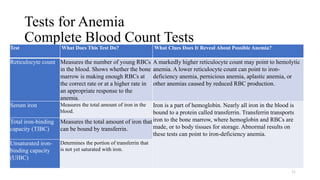
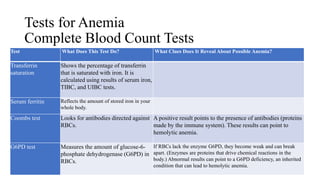
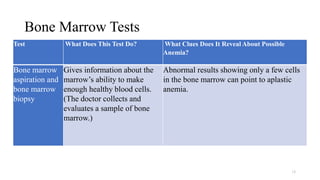
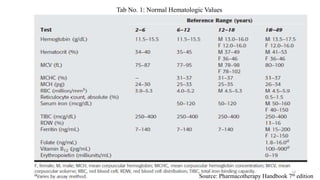
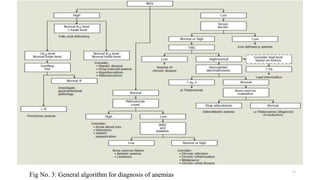
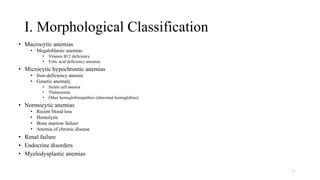
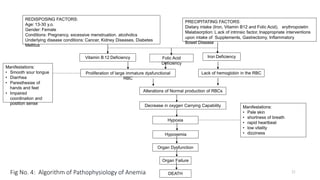
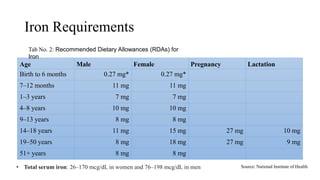
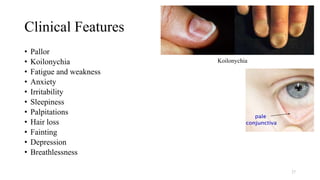
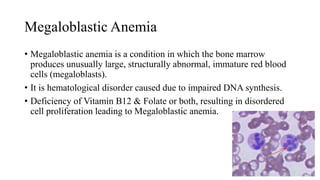
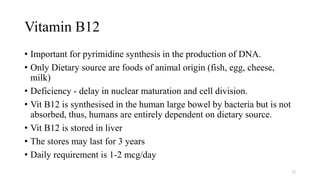
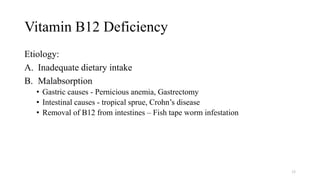
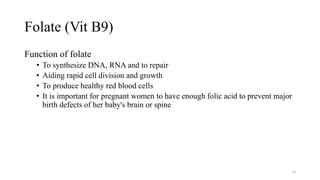
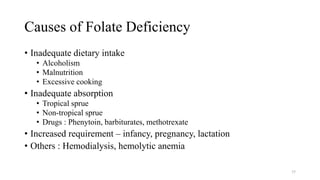
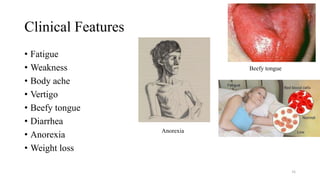
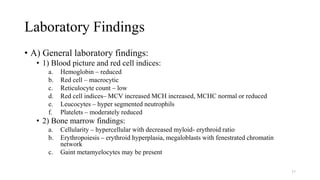
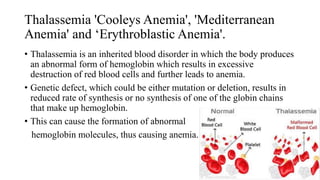
Anemia is a condition where the number of red blood cells or hemoglobin level is lower than normal, resulting in decreased oxygen-carrying capacity of blood. Common causes include blood loss, inadequate red blood cell production, and increased red blood cell destruction. Symptoms include fatigue, weakness, dizziness, and shortness of breath. Diagnosis involves blood tests to measure red blood cell count, hemoglobin level, and other indicators. Specific deficiencies like iron, vitamin B12, or folate can be identified and treated accordingly through diet, supplements, or other means.