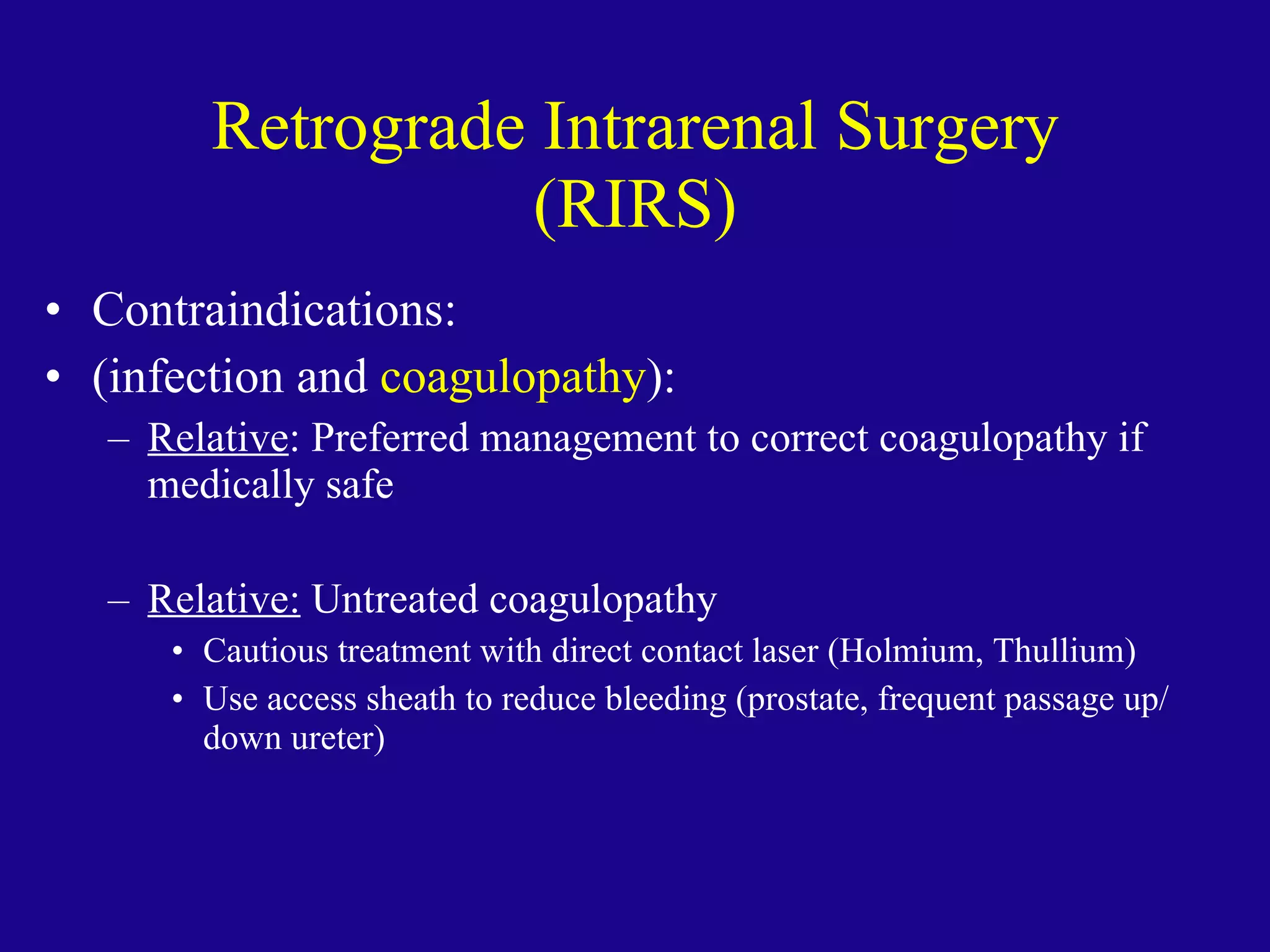
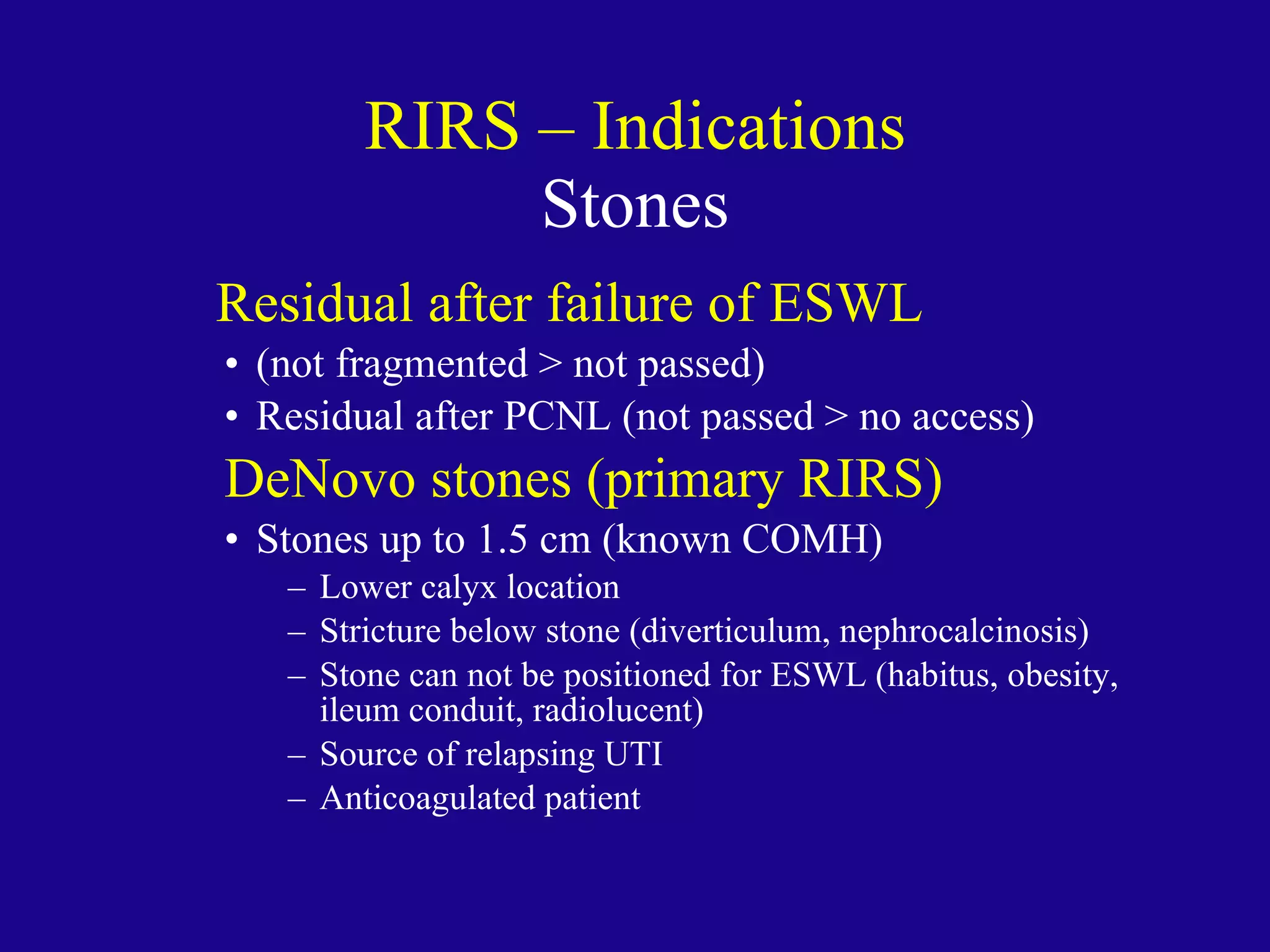
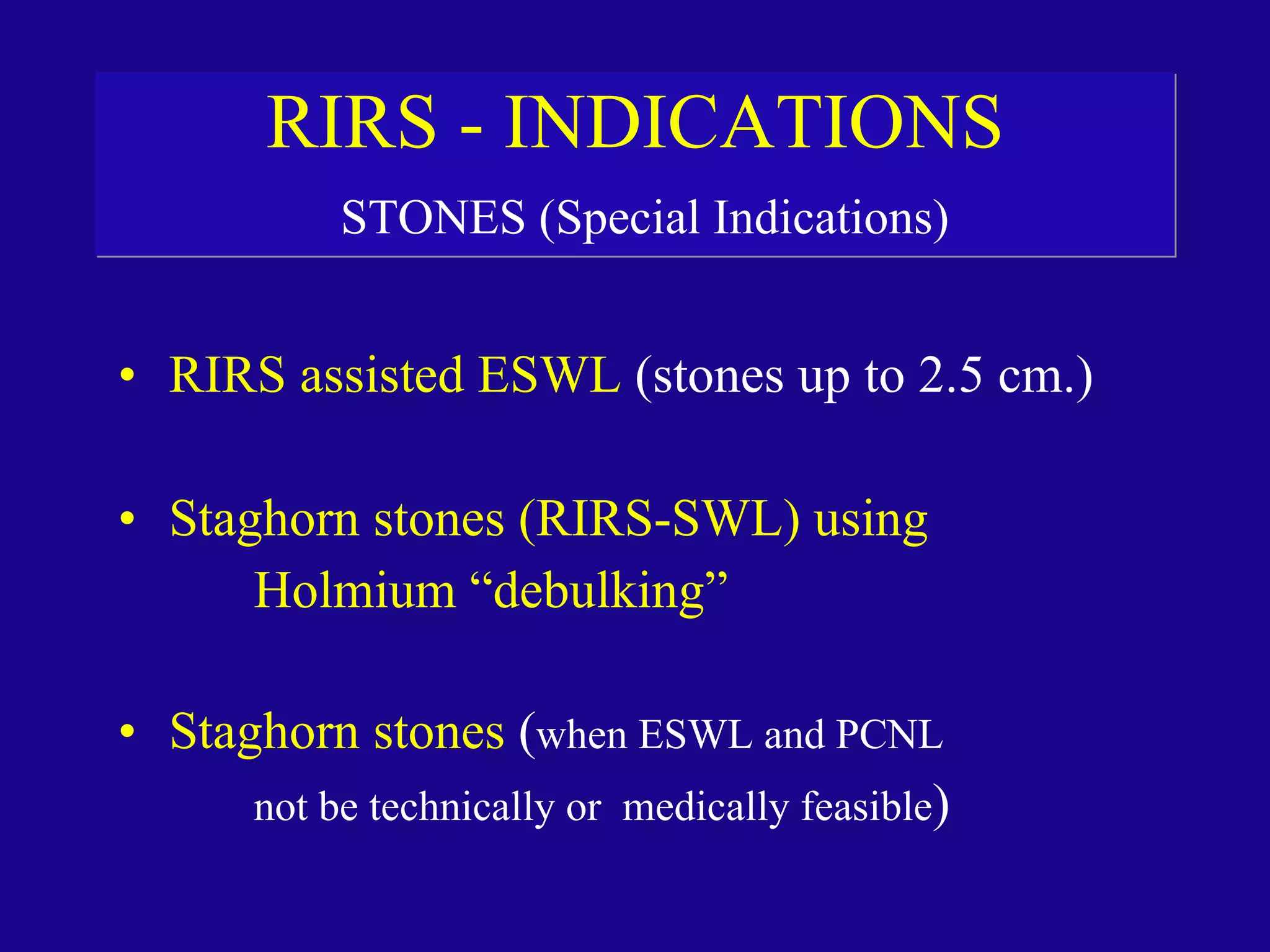
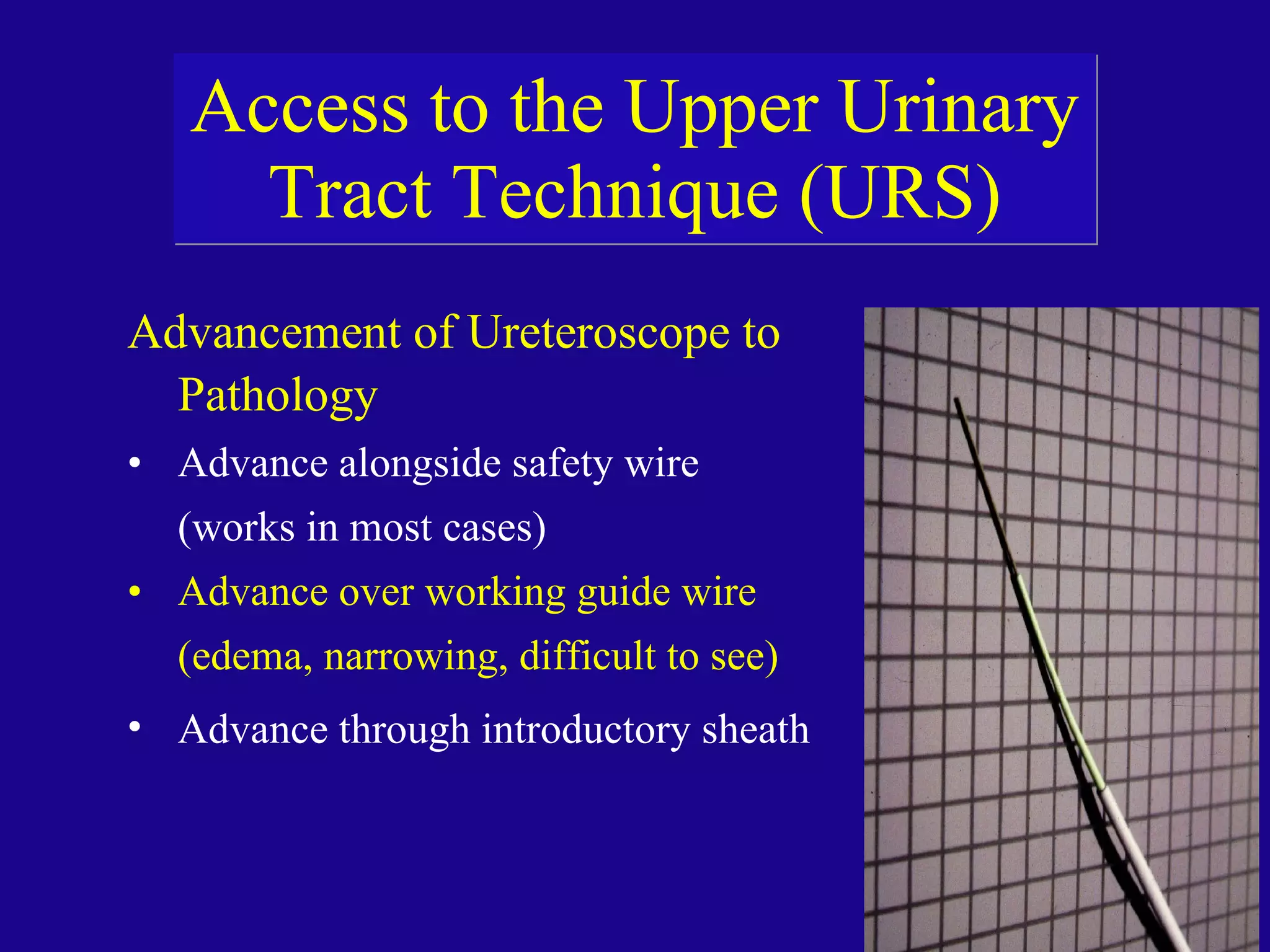
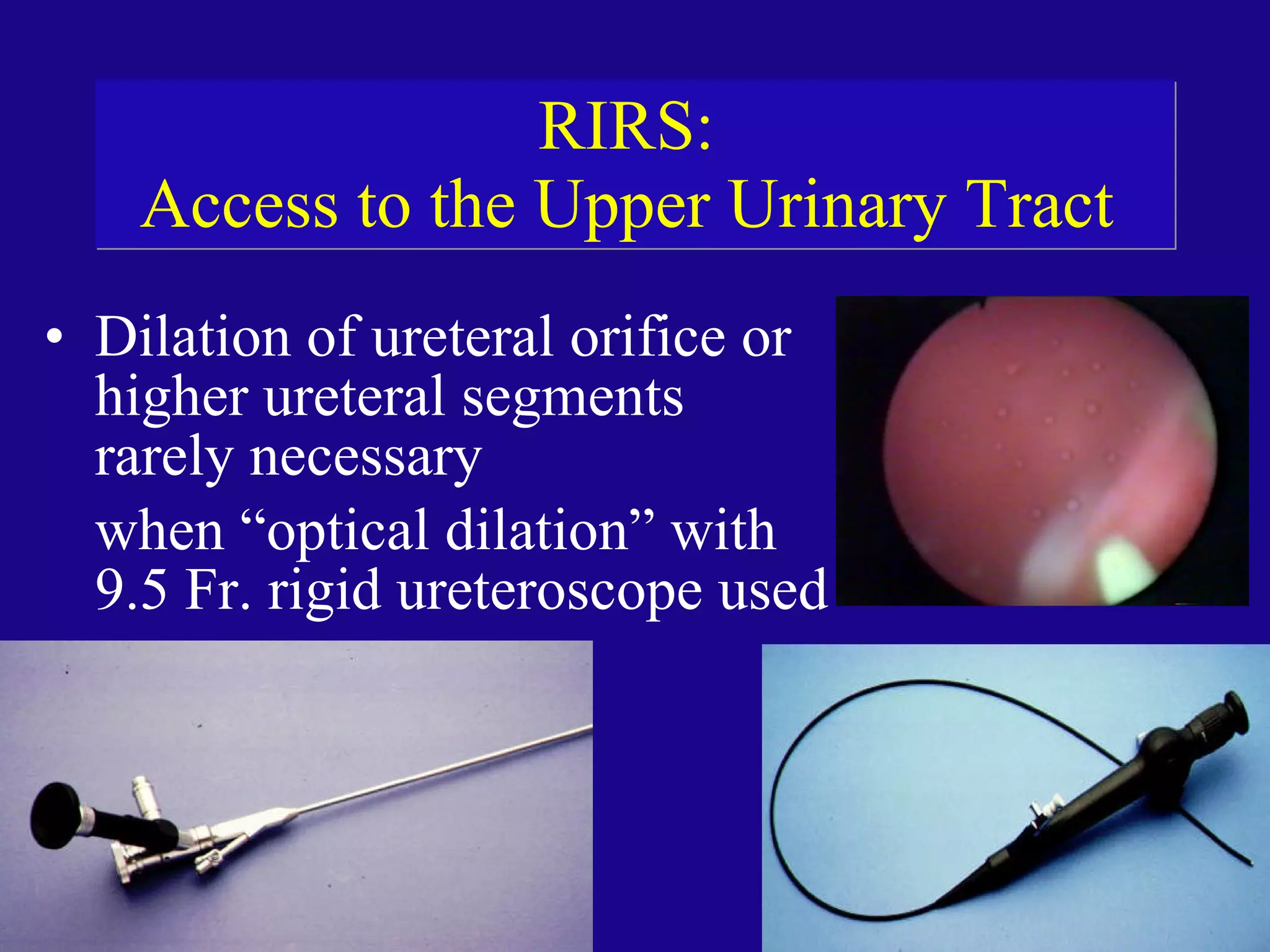
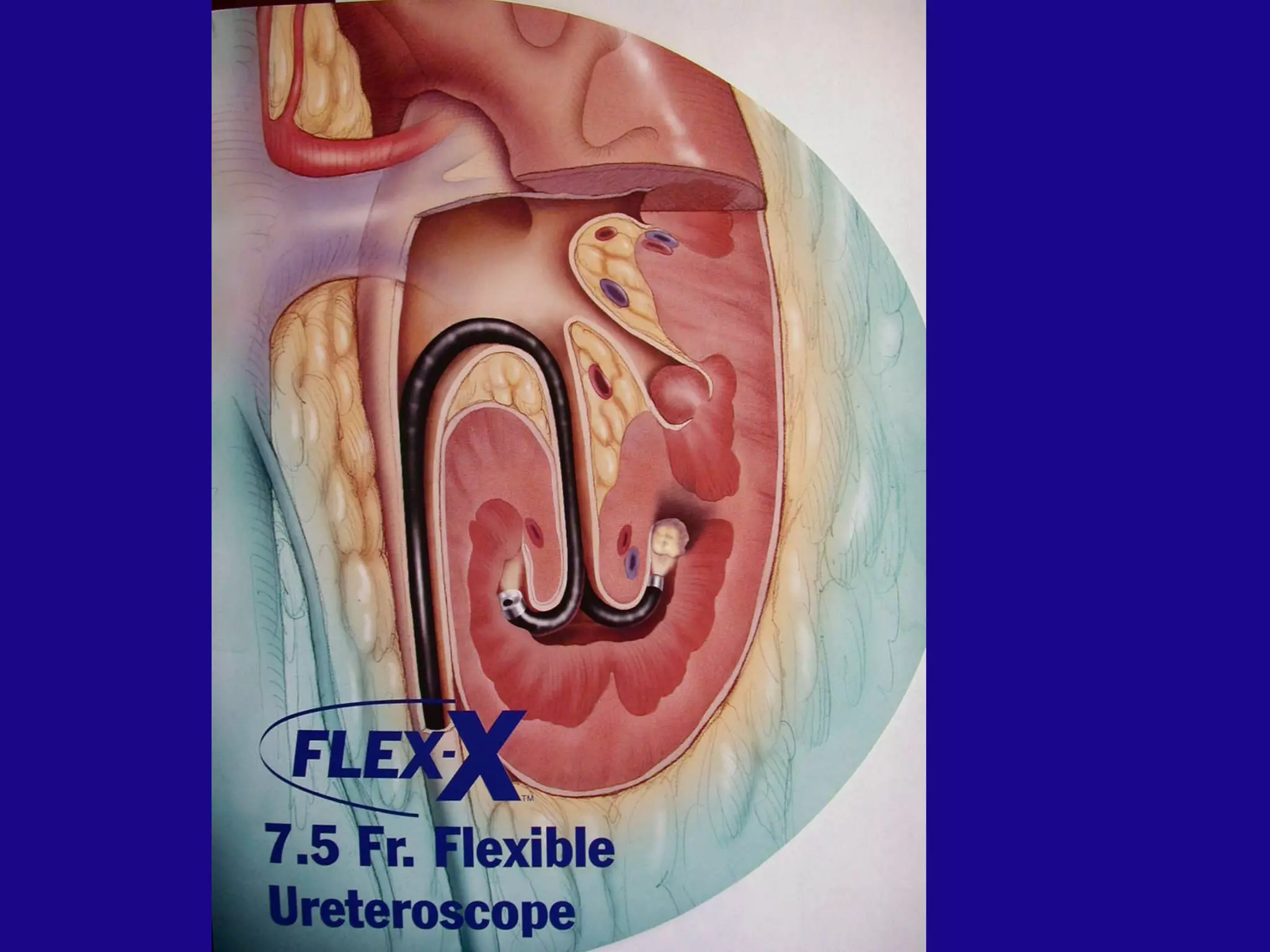
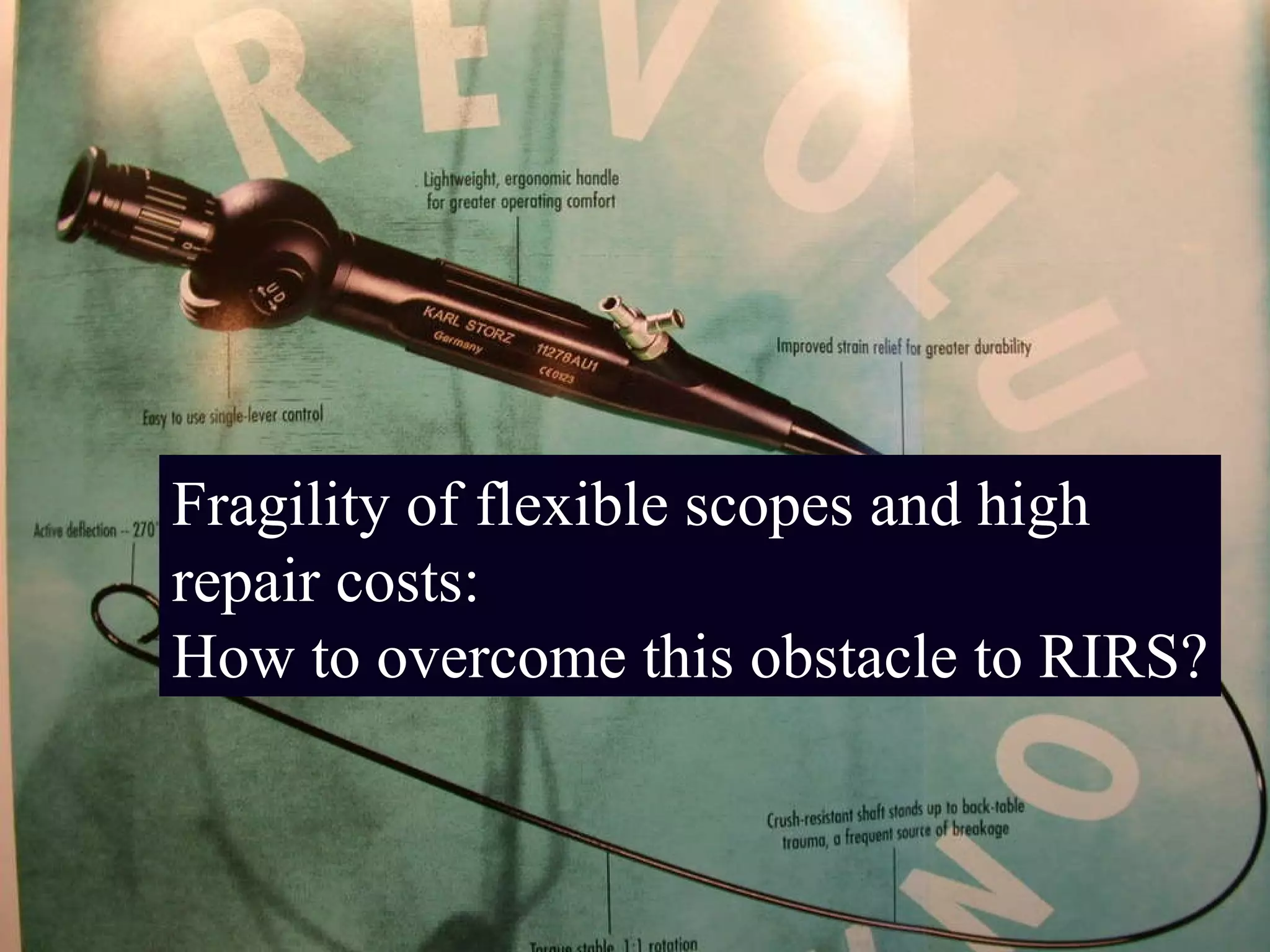
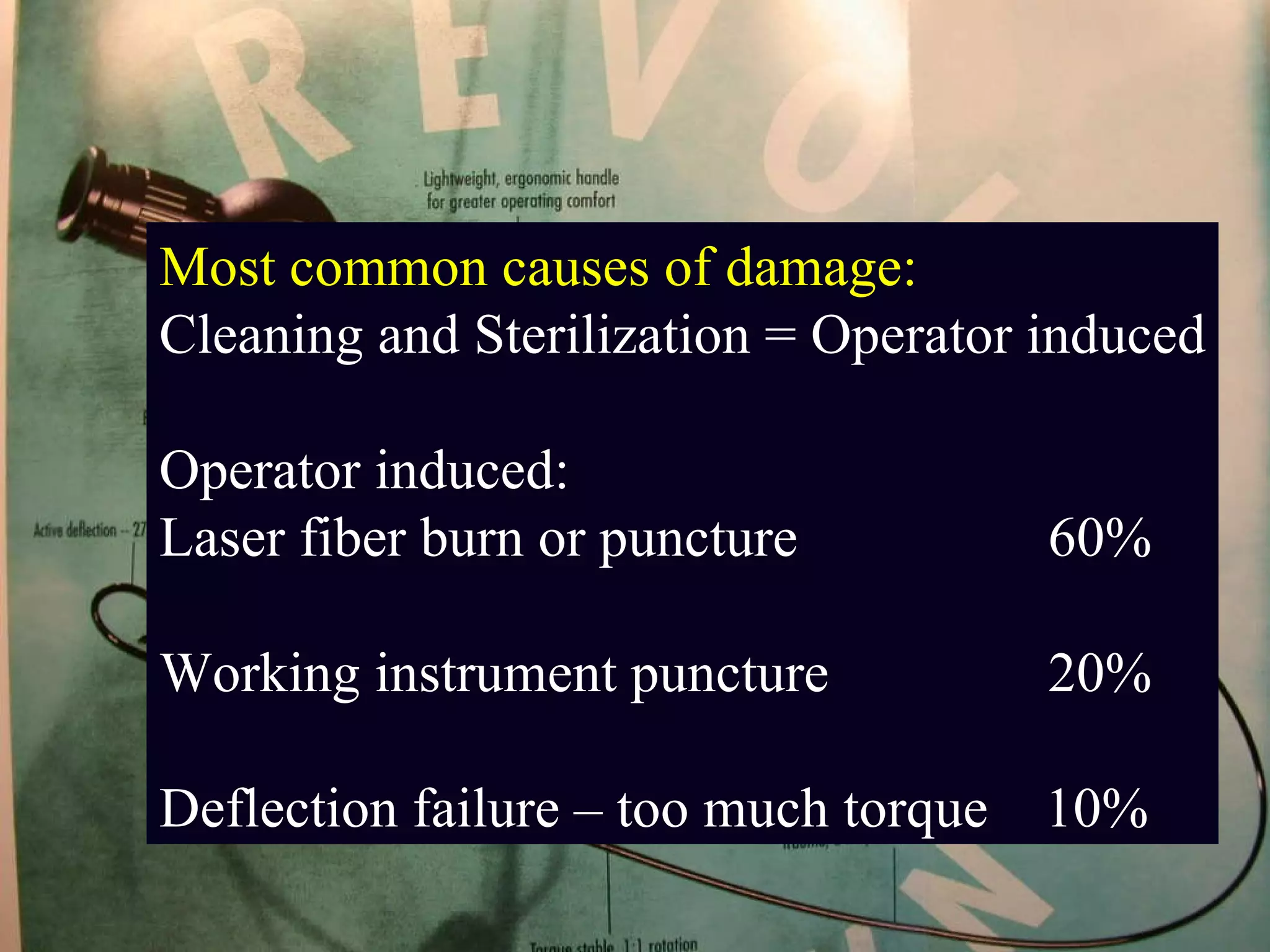
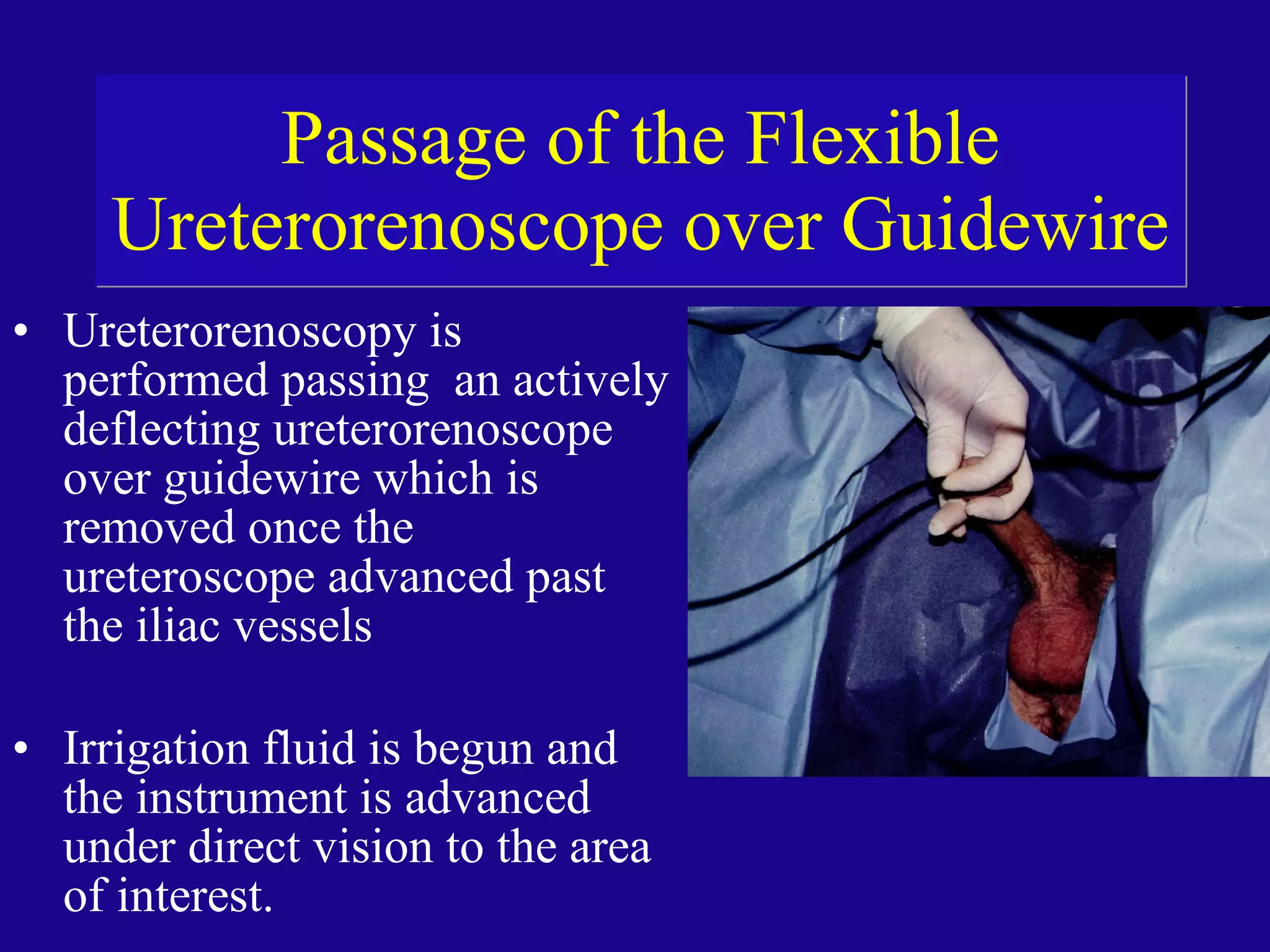
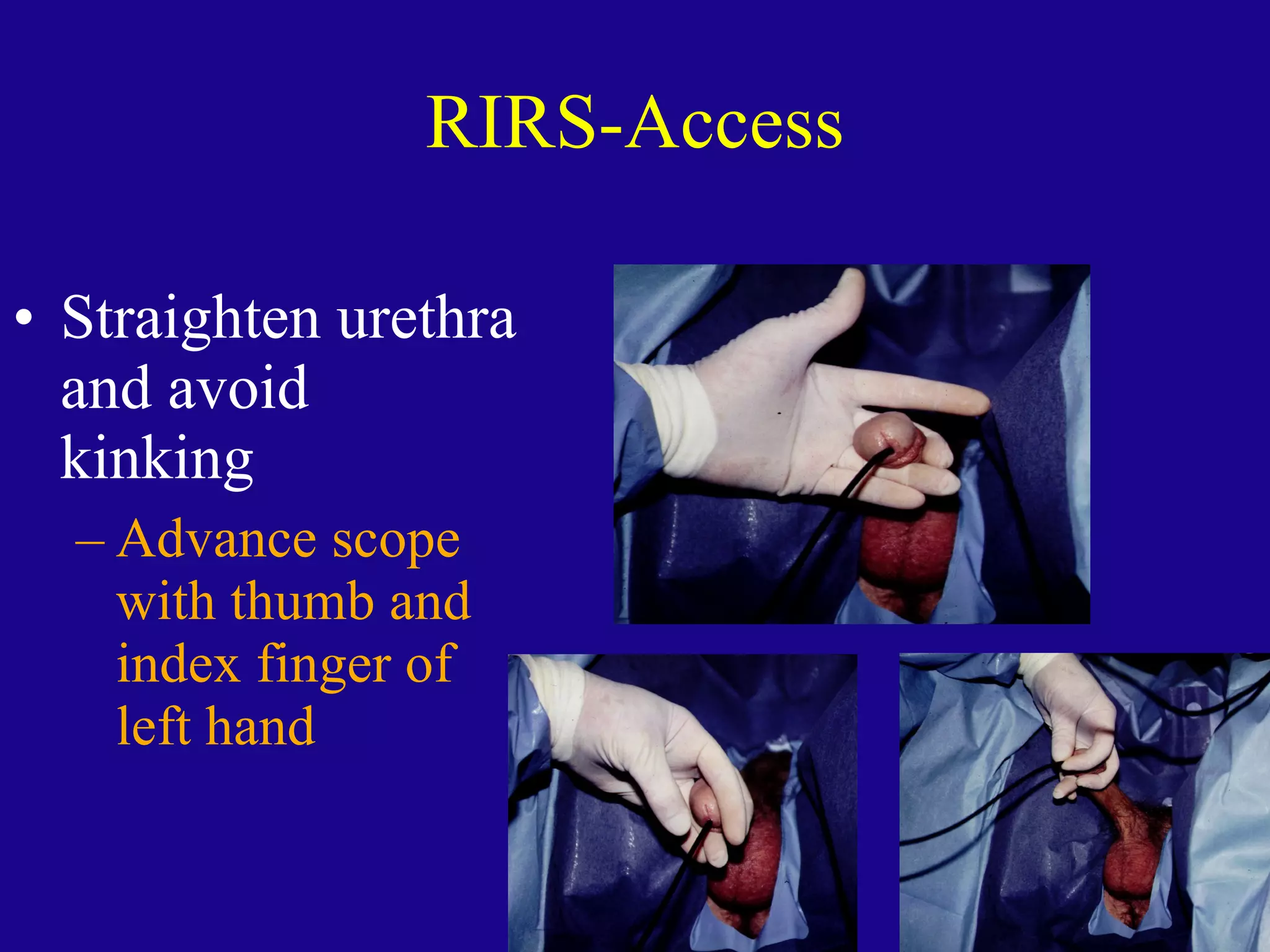
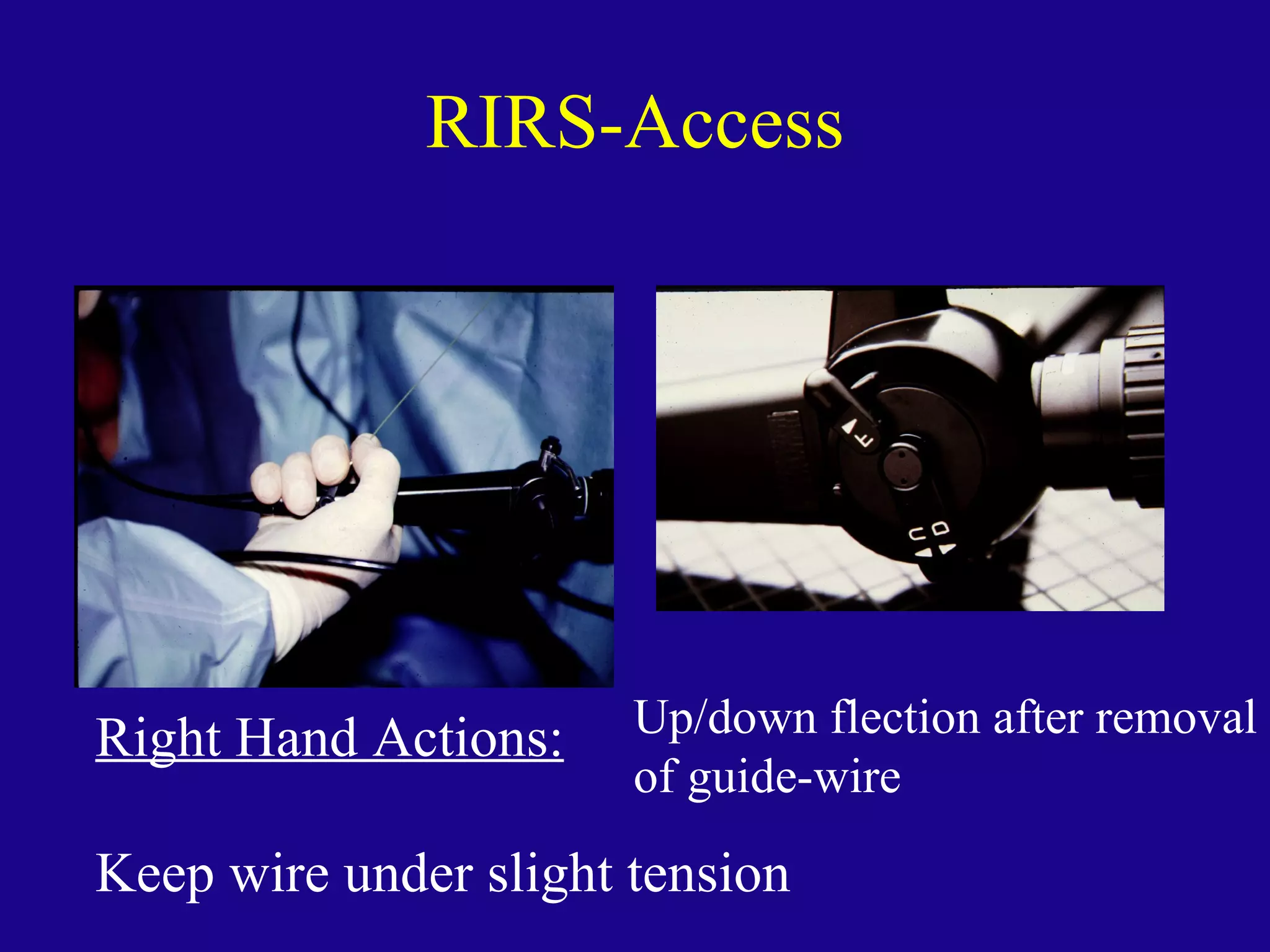
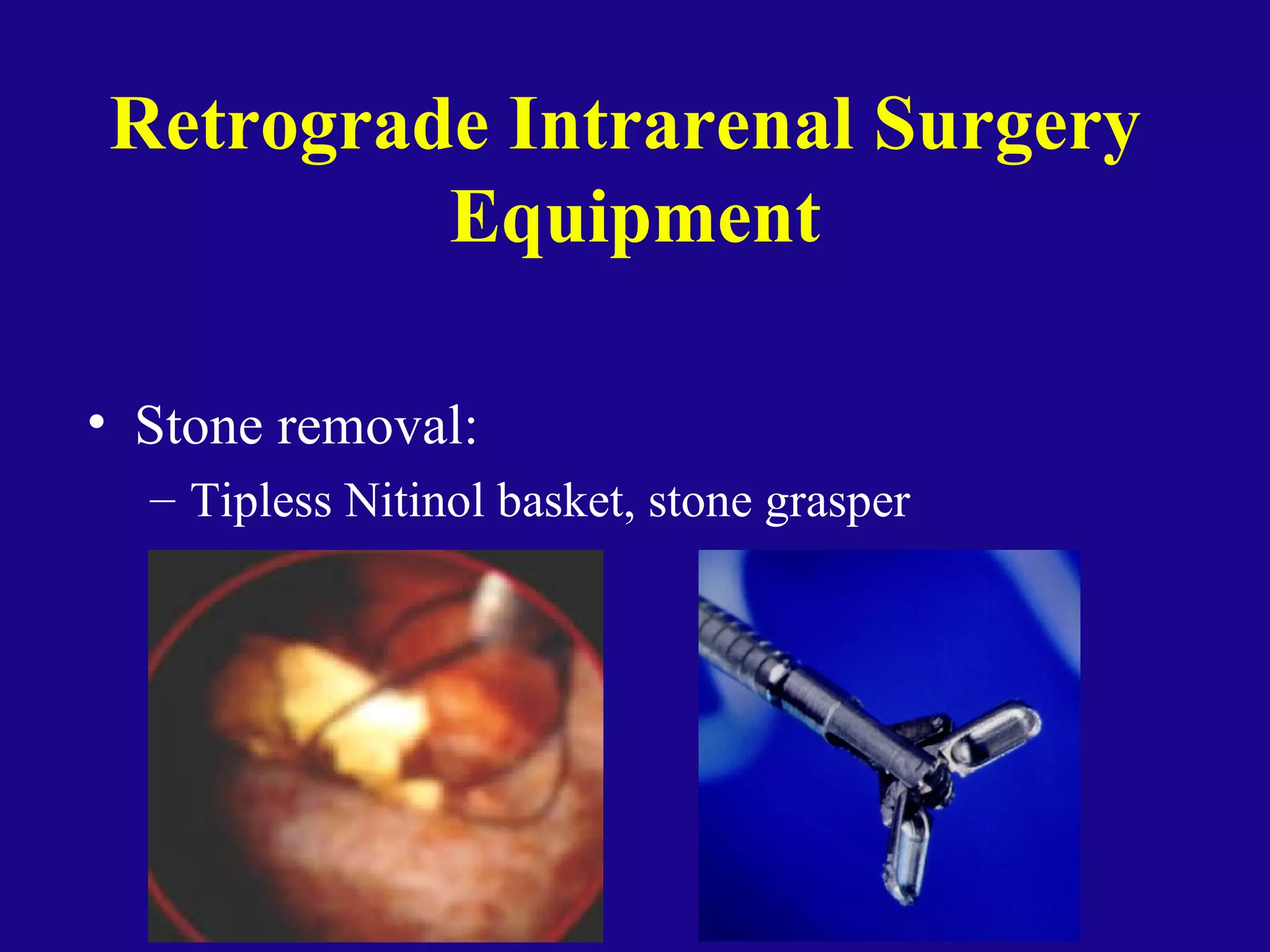
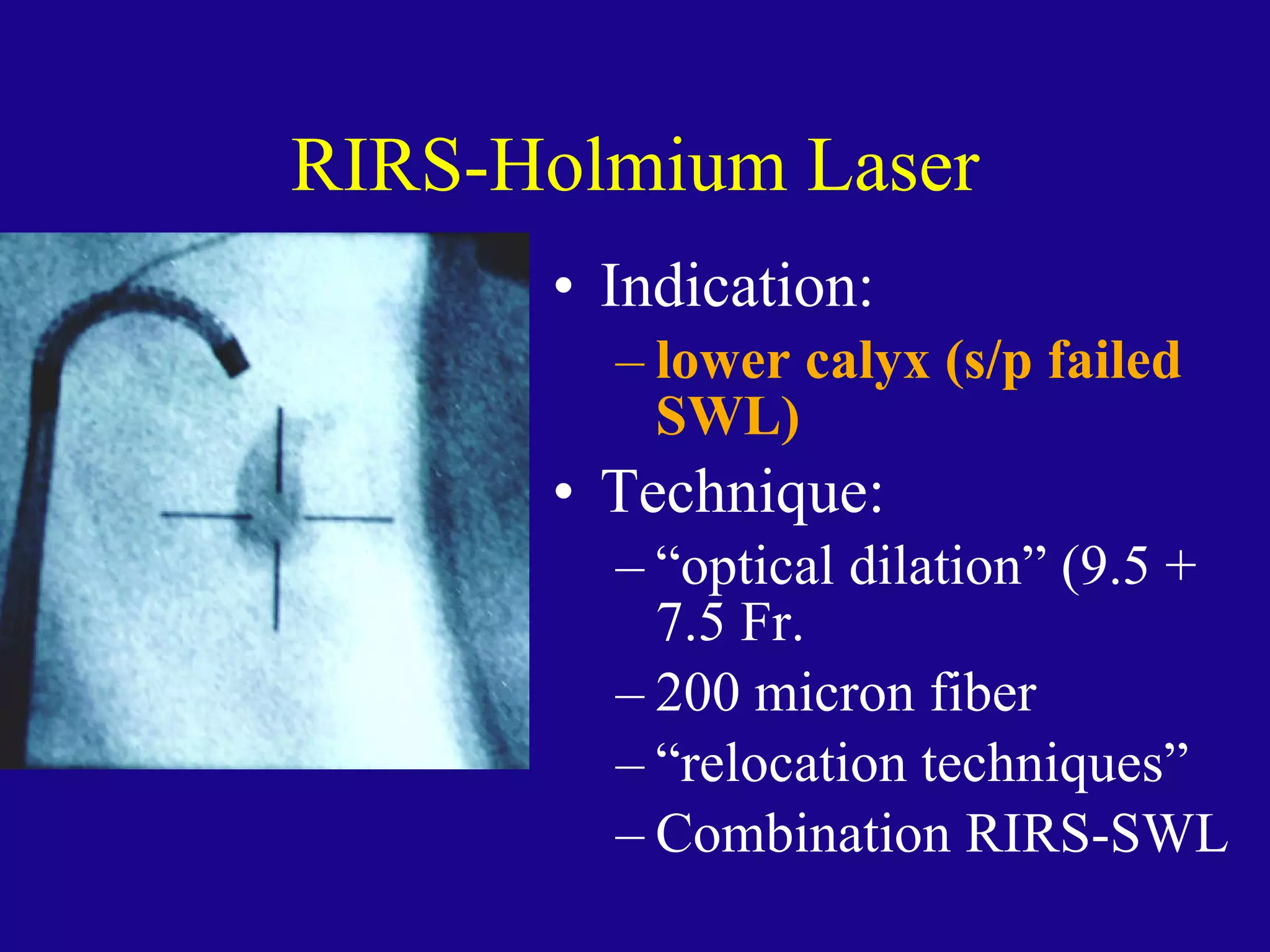
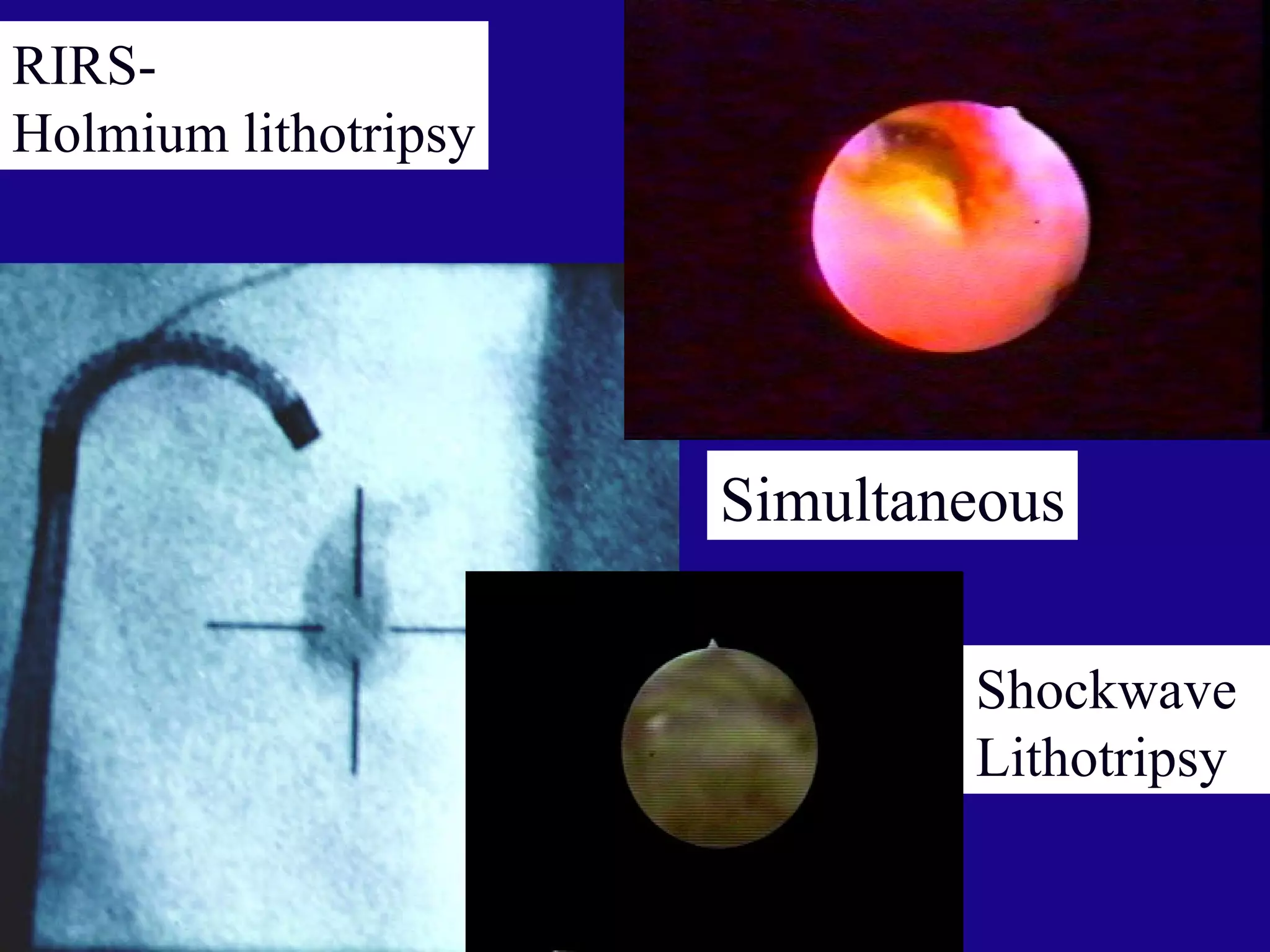
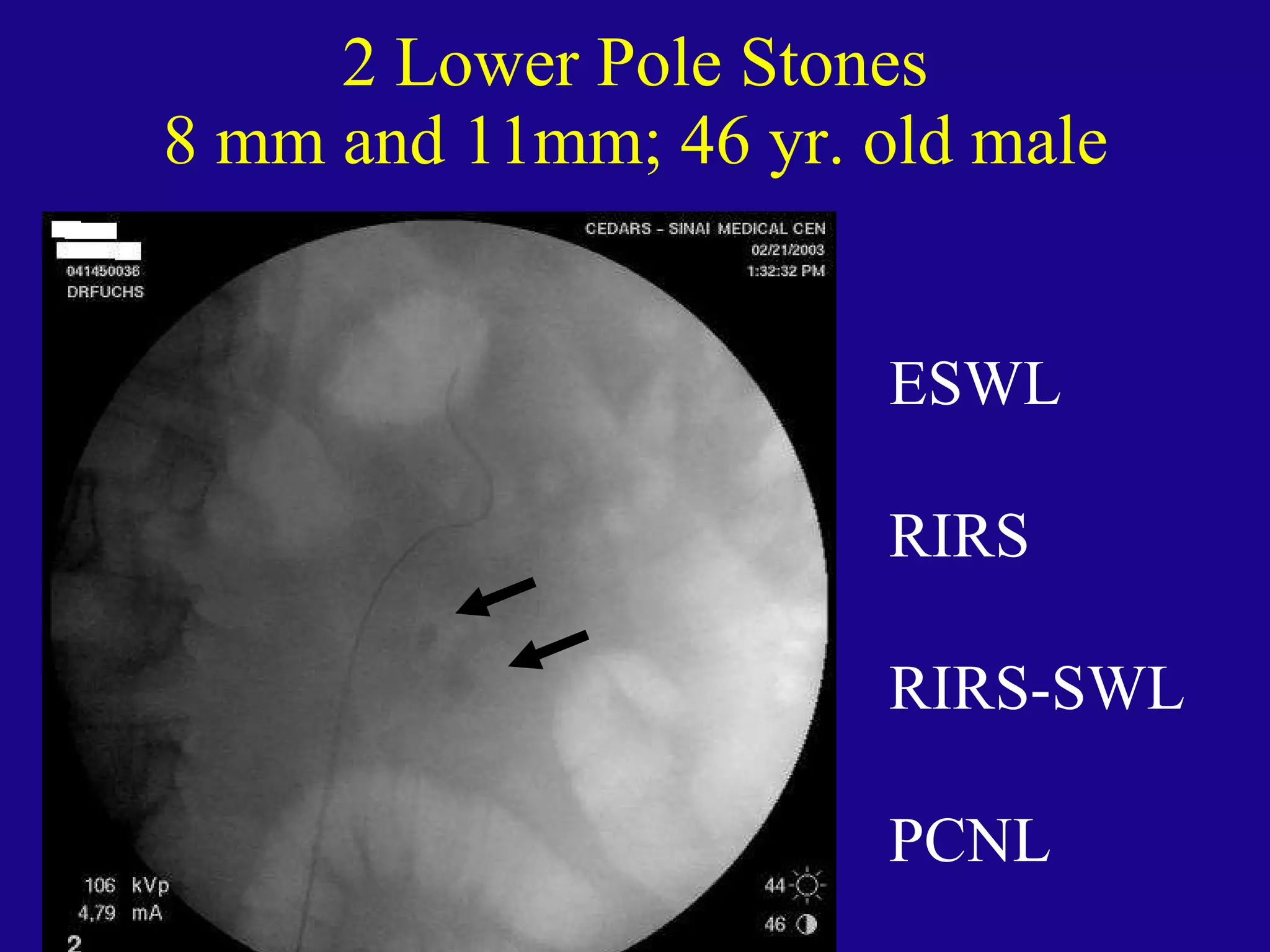
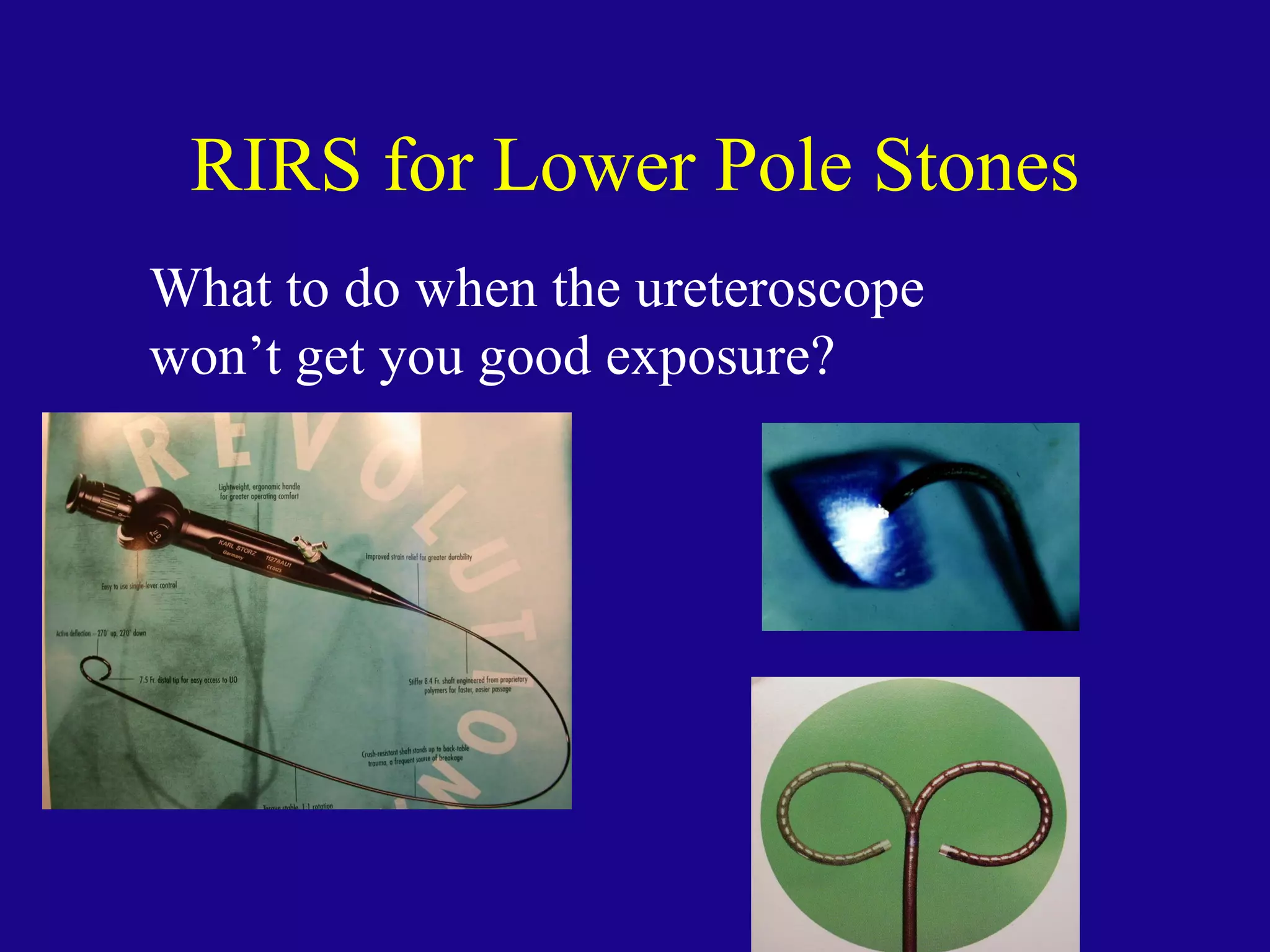
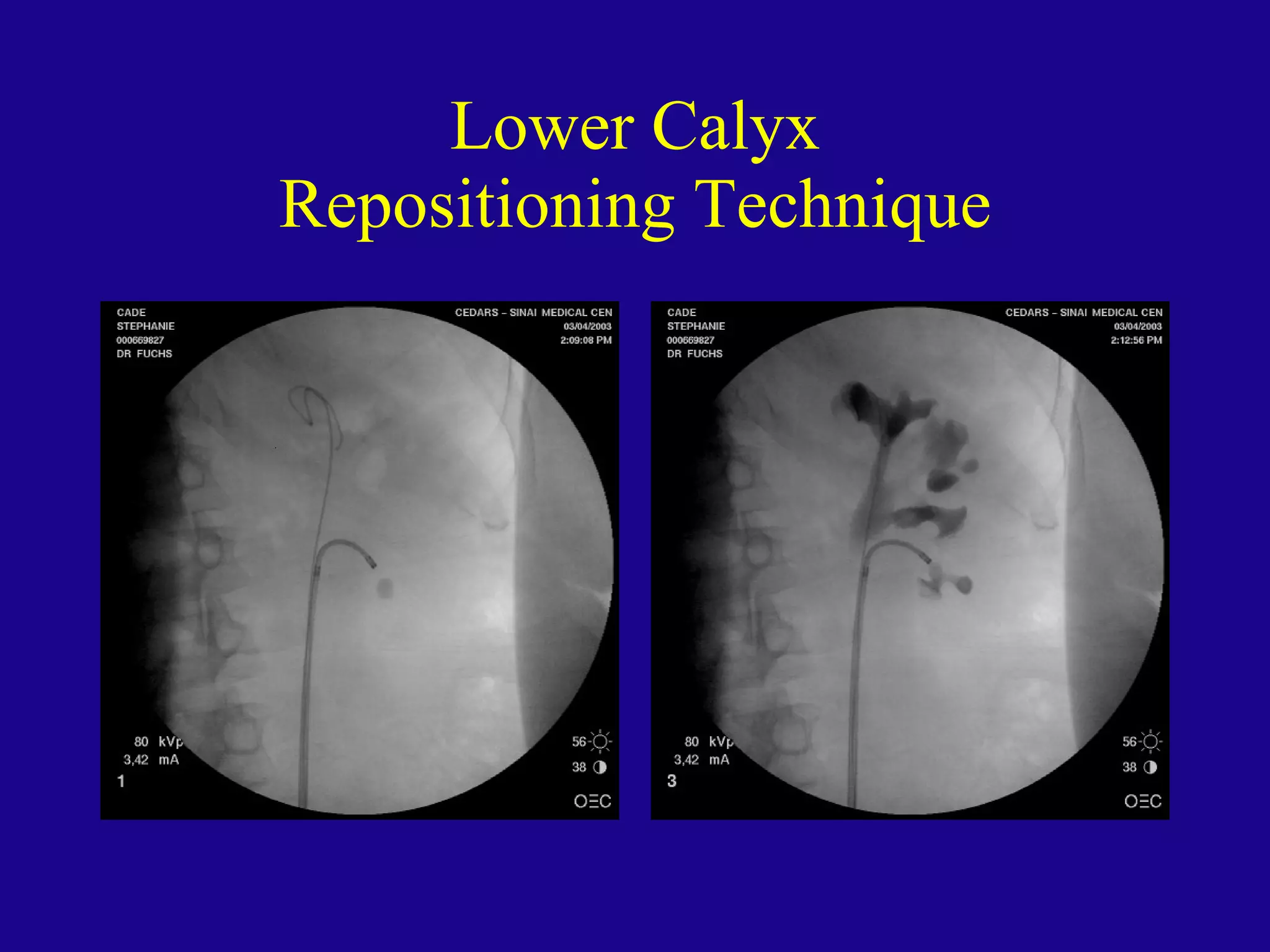
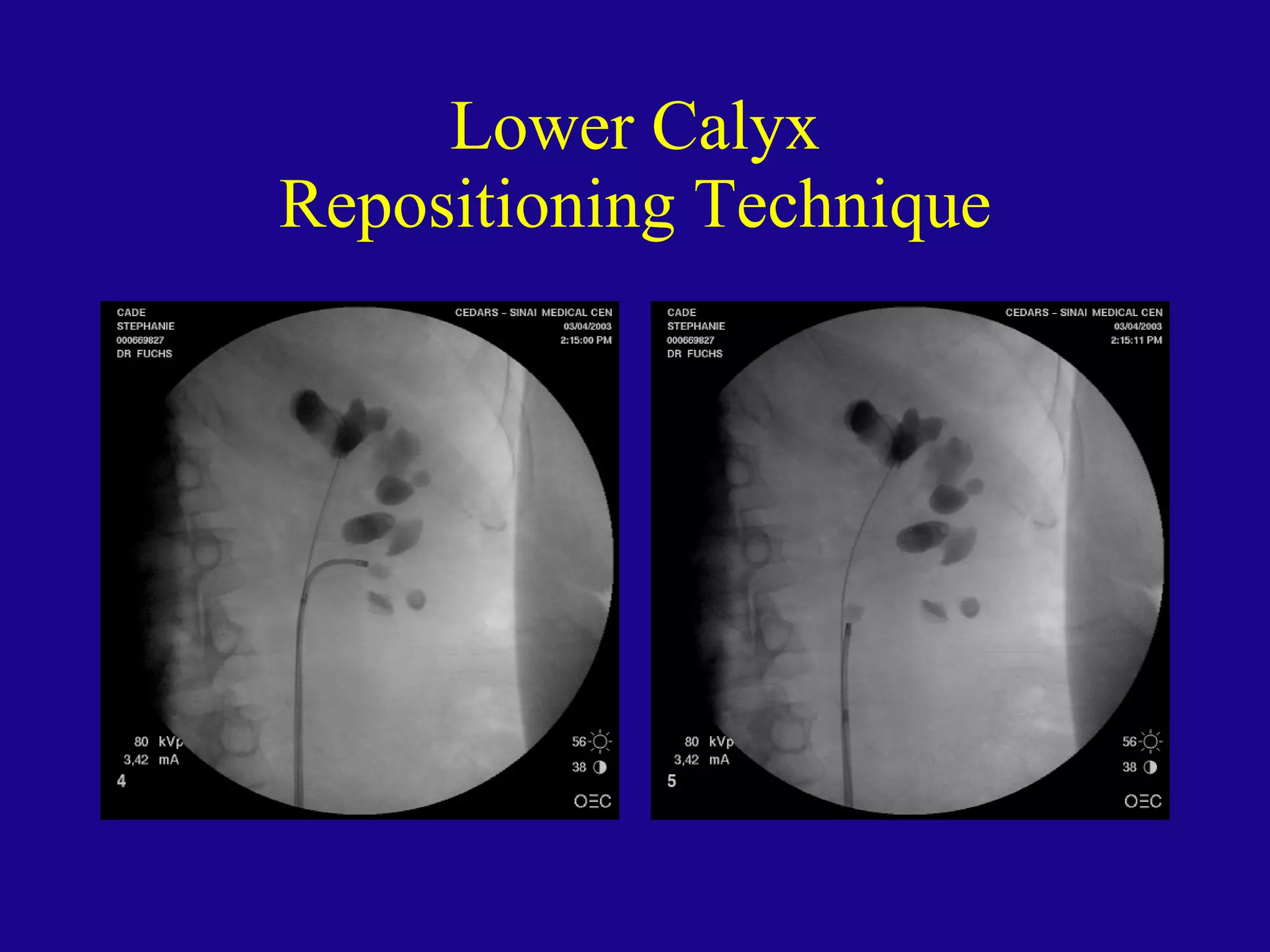
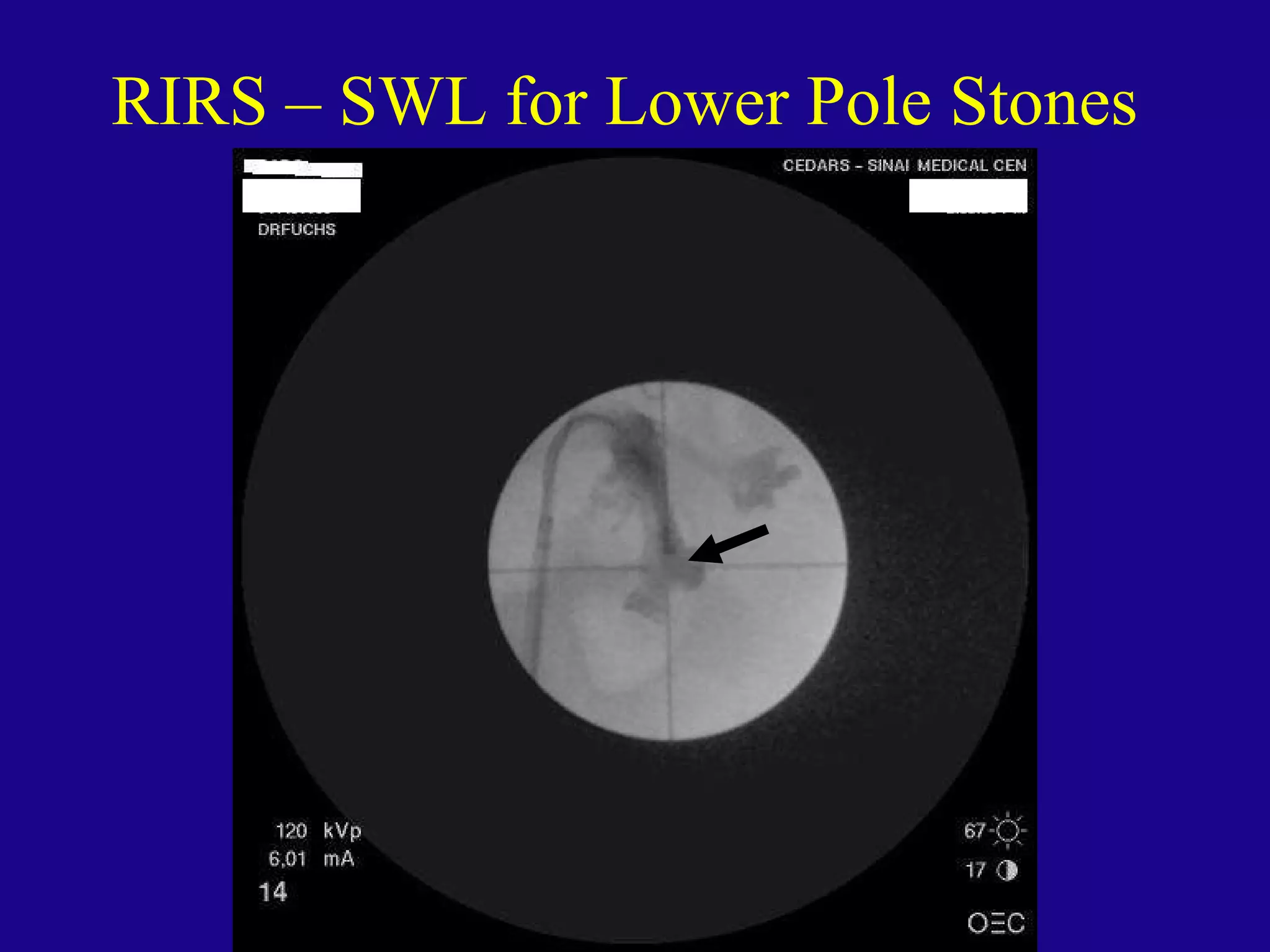
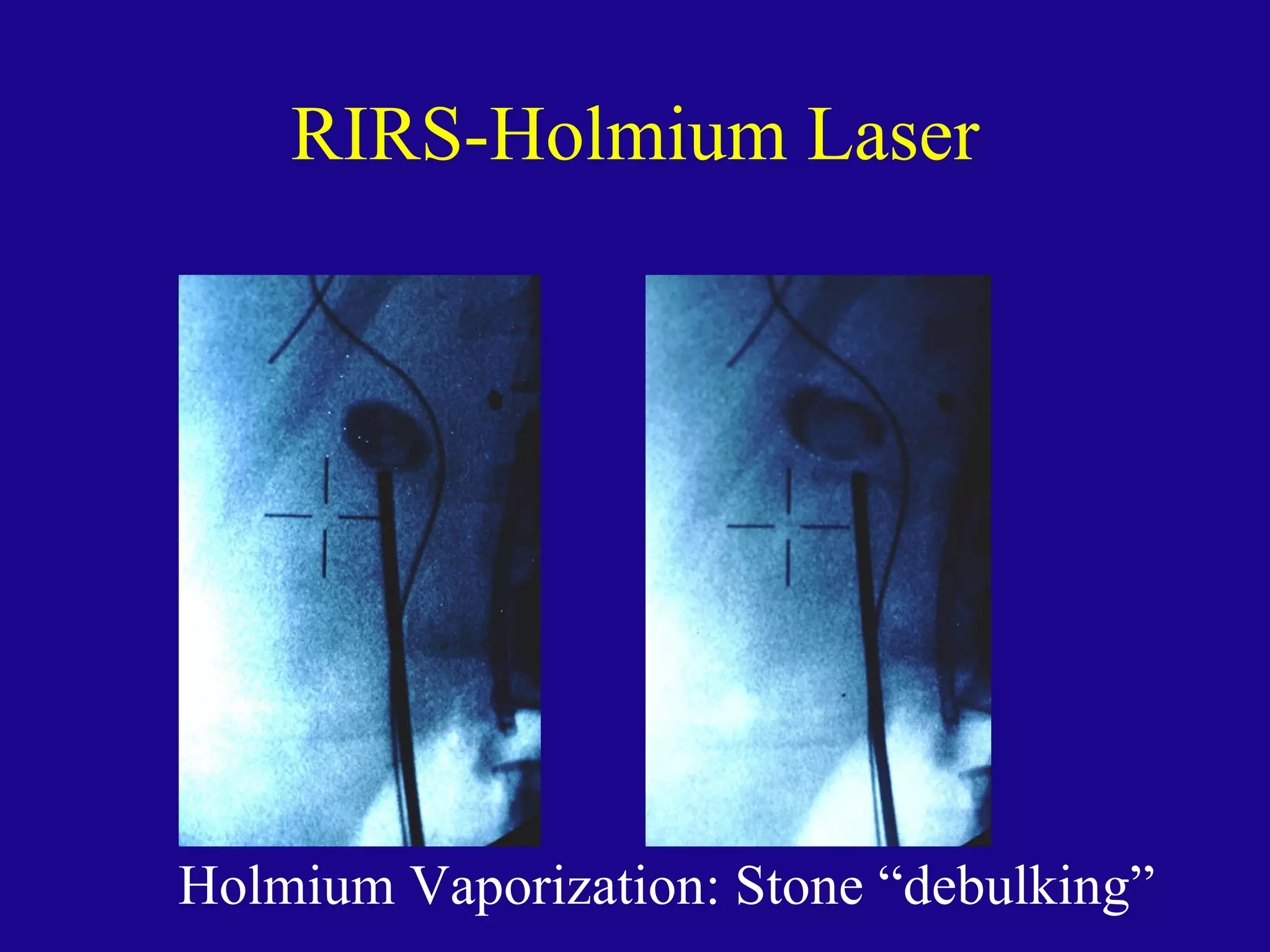
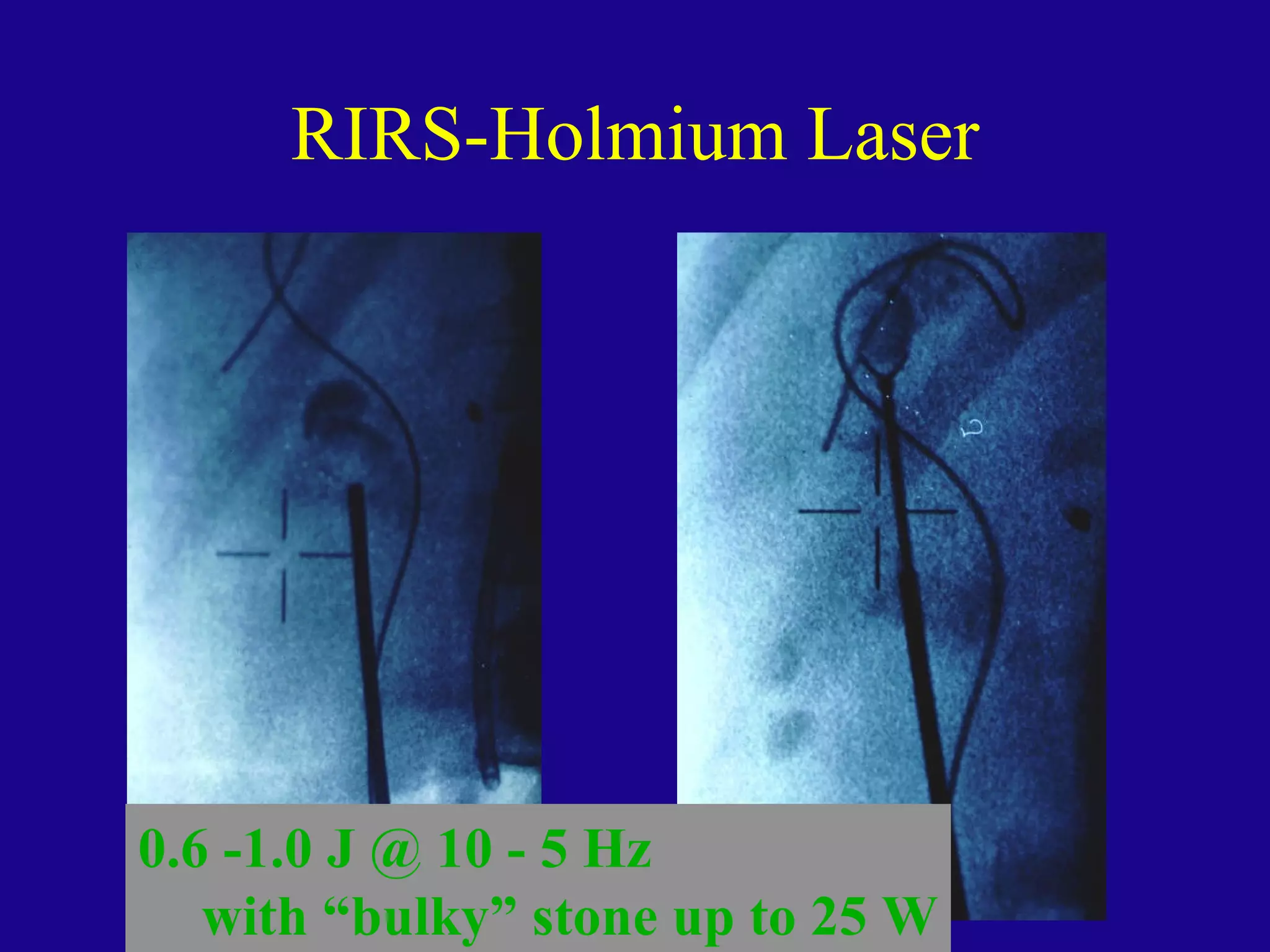
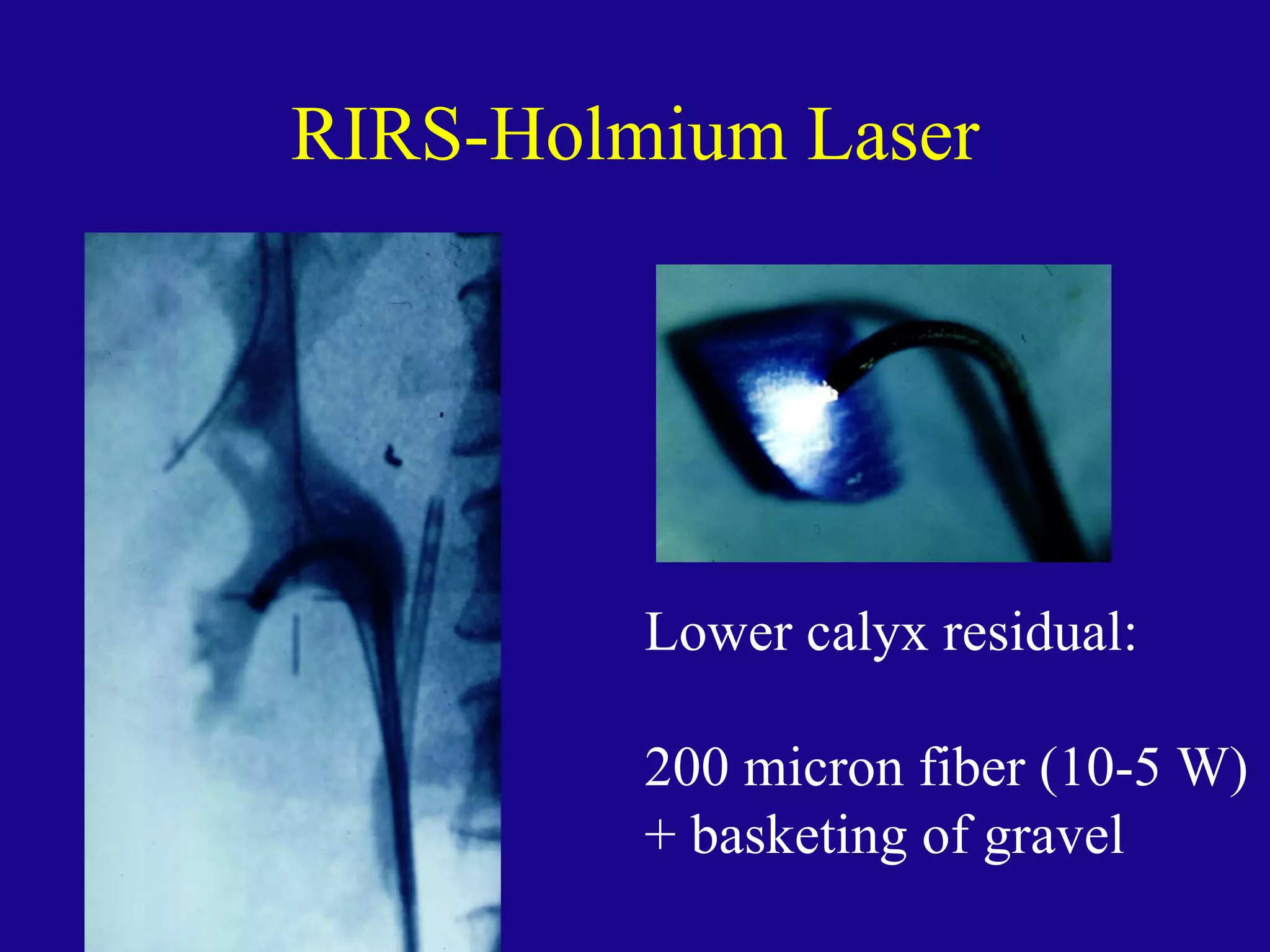
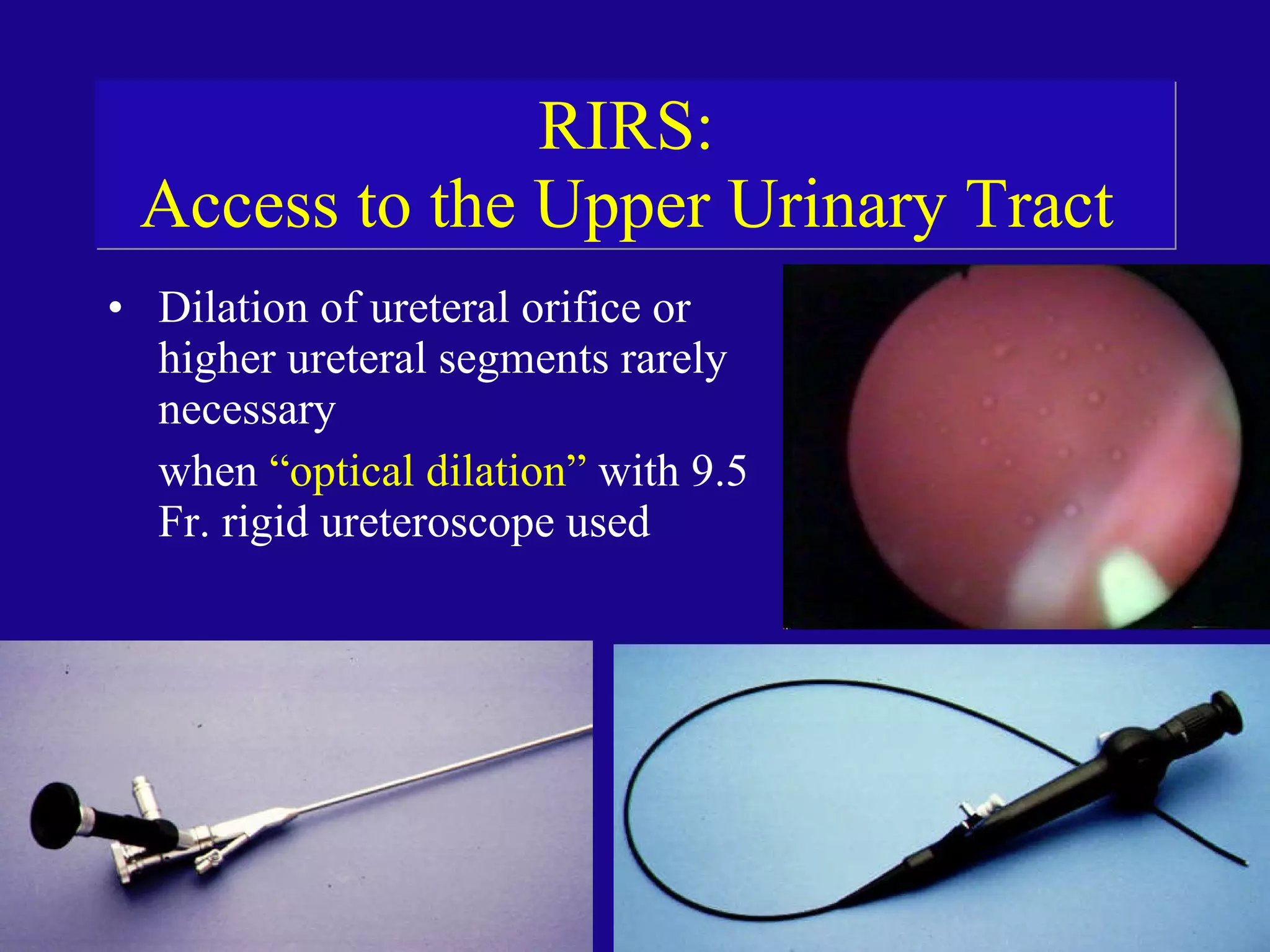
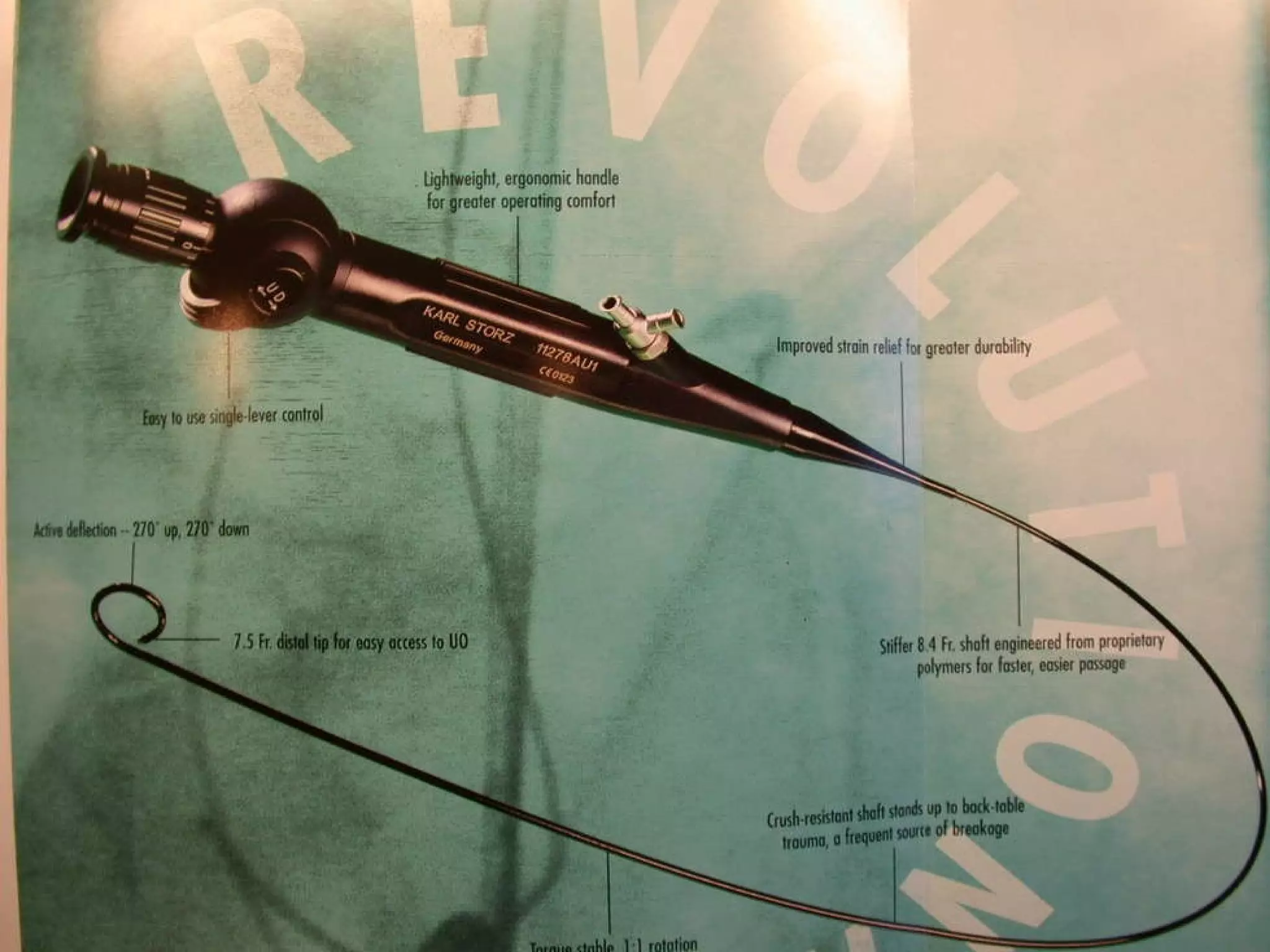
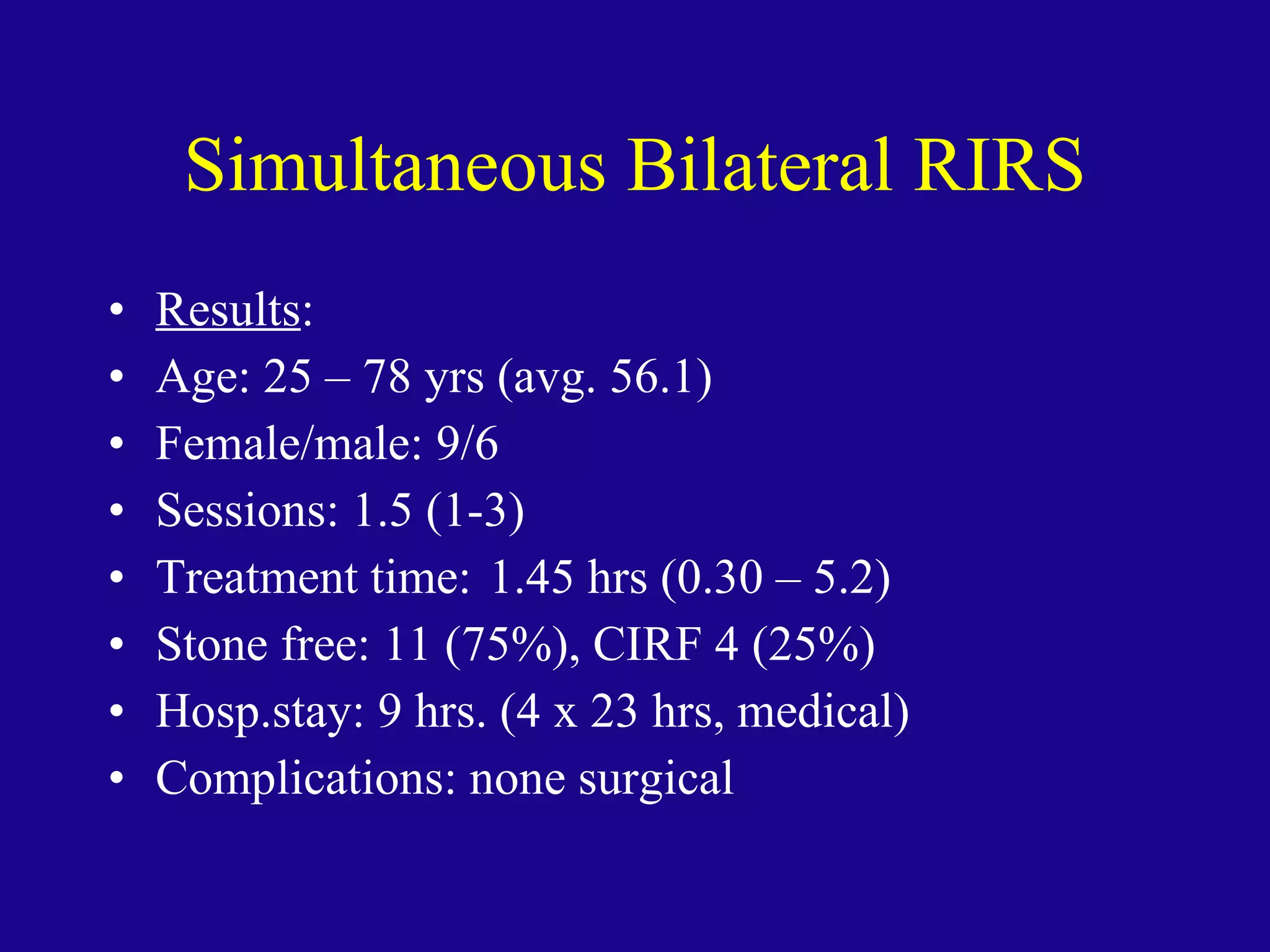
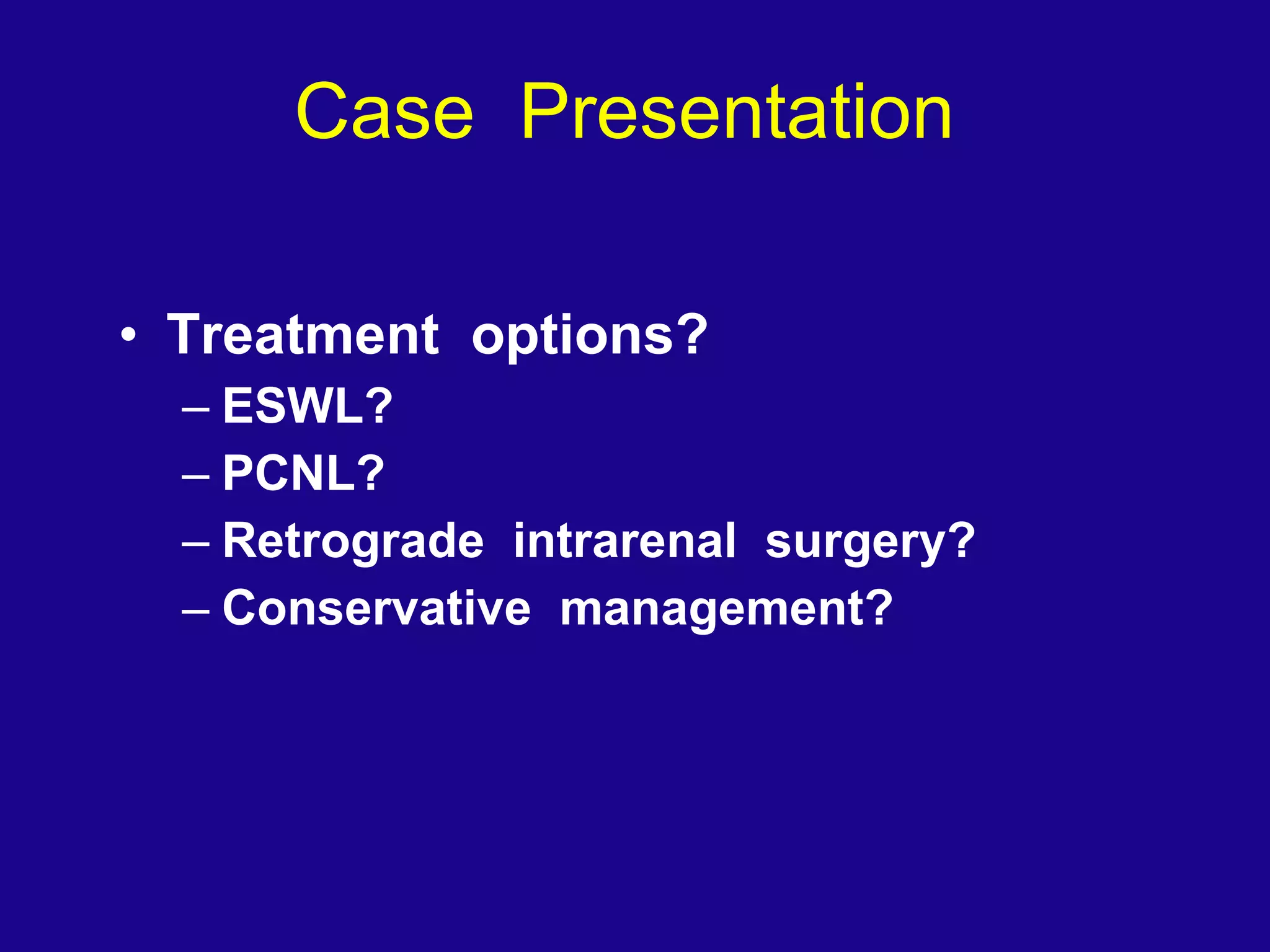
The document outlines a comprehensive overview of retrograde intrarenal ureteroscopic surgery (RIRS), detailing its definitions, contraindications, indications for use, techniques, and outcomes. It discusses advancements in equipment and instrumentation, patient preparation, and clinical case examples illustrating RIRS in various scenarios including stone management and tumor treatment. The future outlook for RIRS reveals its growing role in the minimally invasive treatment for urological conditions, increasingly replacing traditional methods like SWL and PCNL.
































































































































































![RIRS –Endourology Info [email_address] Fax: 310 423 4711 Ph: 310 423 4700](https://image.slidesharecdn.com/fuchs-rirs-saopaulo-08-110331094215-phpapp02/75/Retrograde-Intrarenal-Ureteroscopic-Surgery-RIRS-203-2048.jpg)