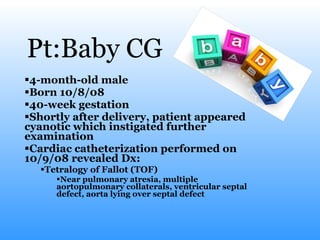
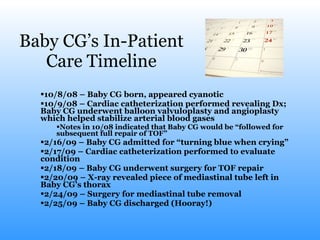
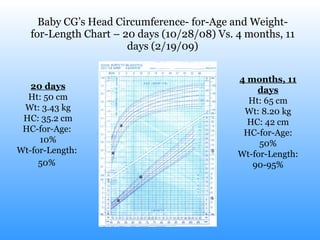
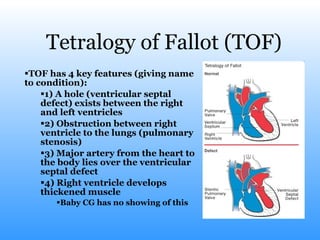
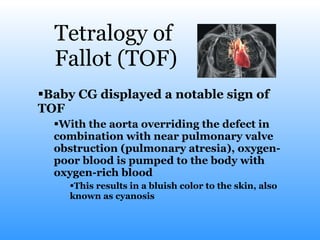
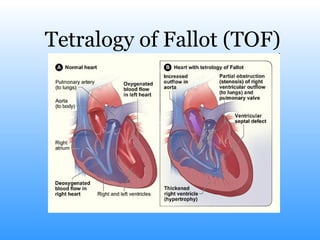
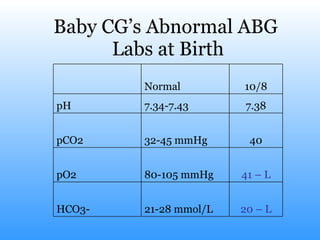
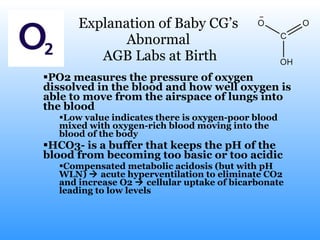
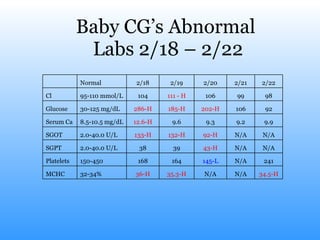
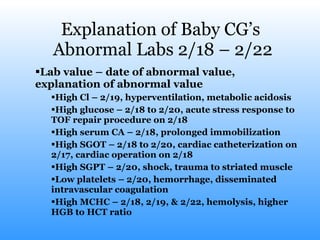
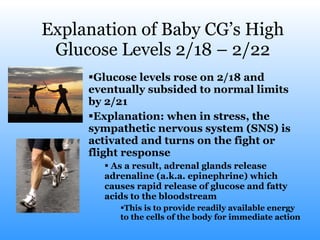
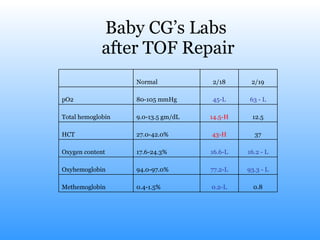
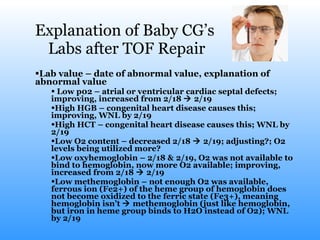
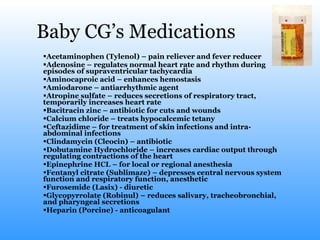
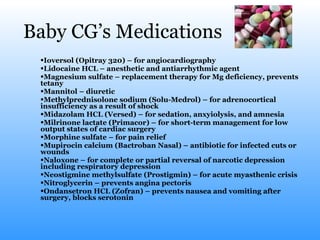
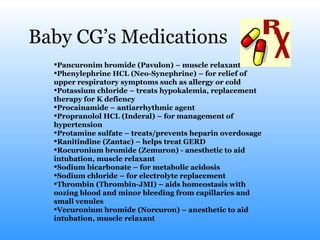
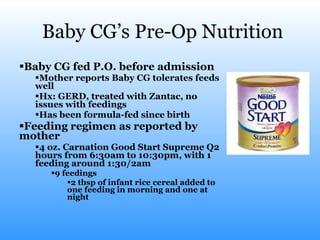
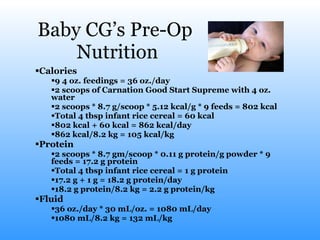
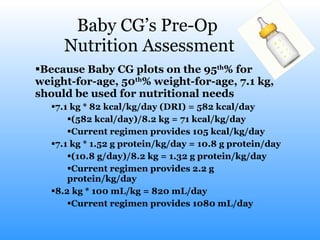
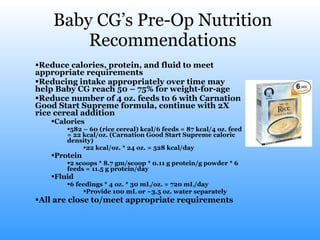
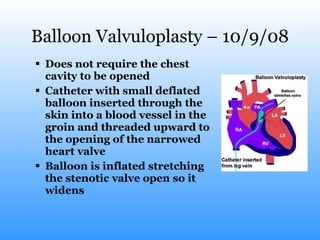
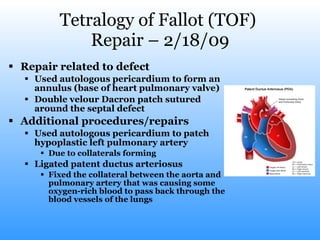
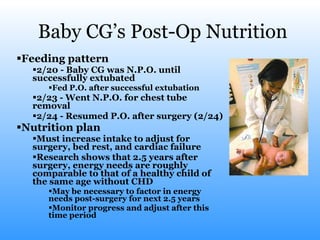
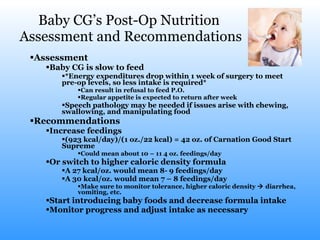
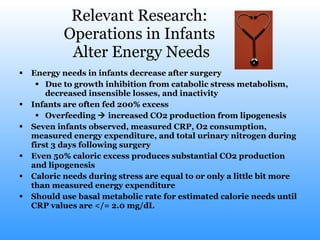
The document describes a pediatric case study of a 4-month-old male, Baby CG, born with Tetralogy of Fallot (TOF). Baby CG underwent various procedures including balloon valvuloplasty, angioplasty, and full TOF repair surgery. Baby CG's labs showed abnormalities including low oxygen levels and high glucose levels after surgery, which improved over time. The document also details Baby CG's medications, nutrition, and growth charts pre- and post-operatively.