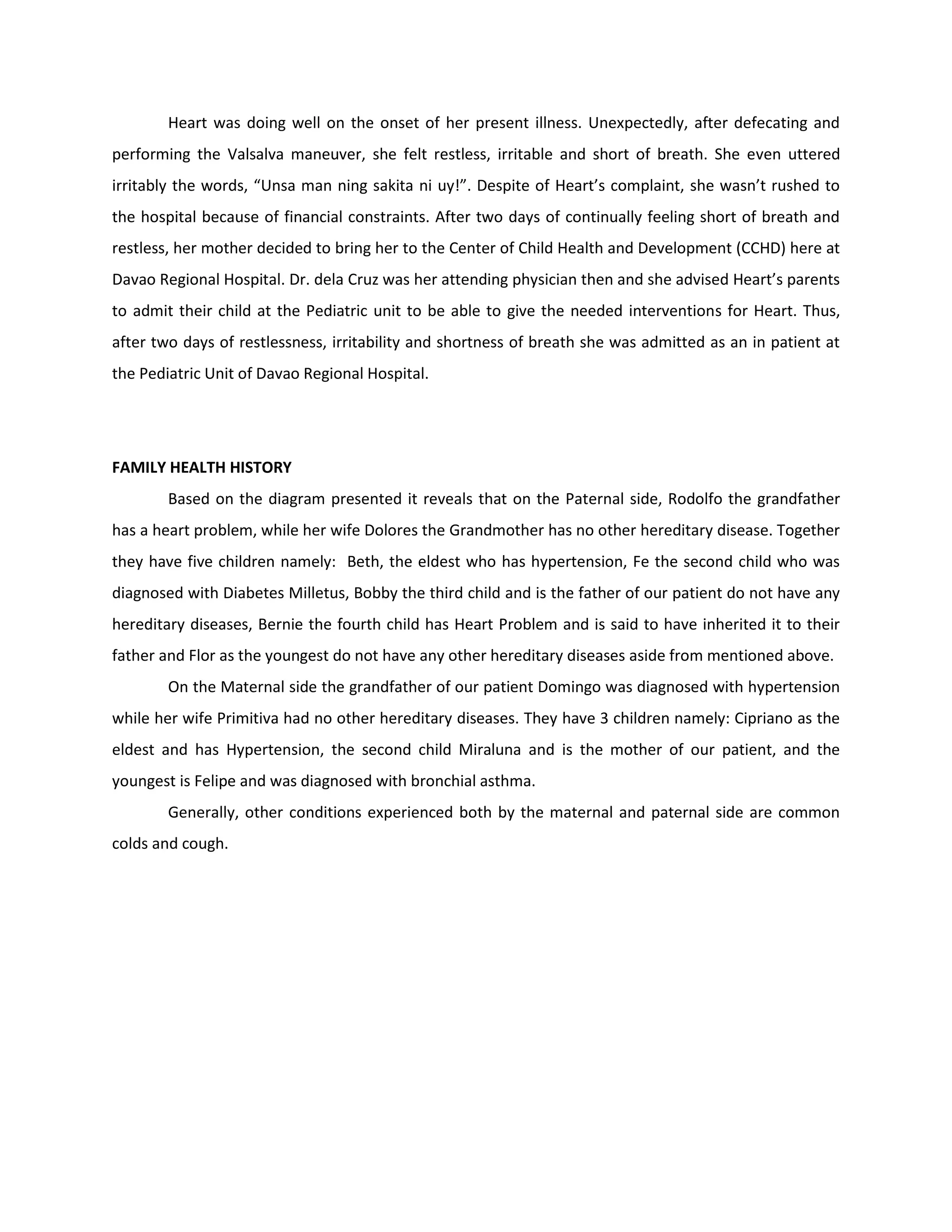
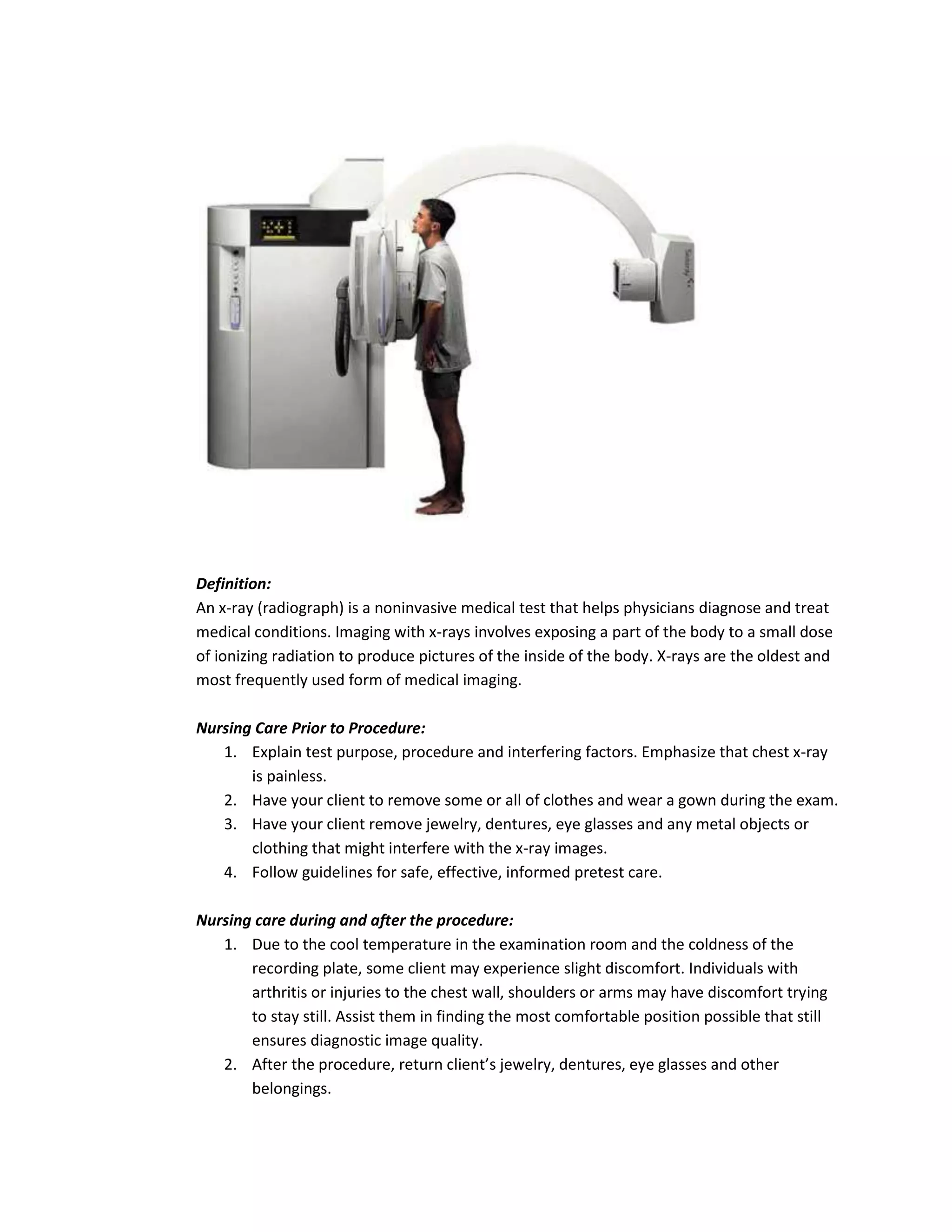
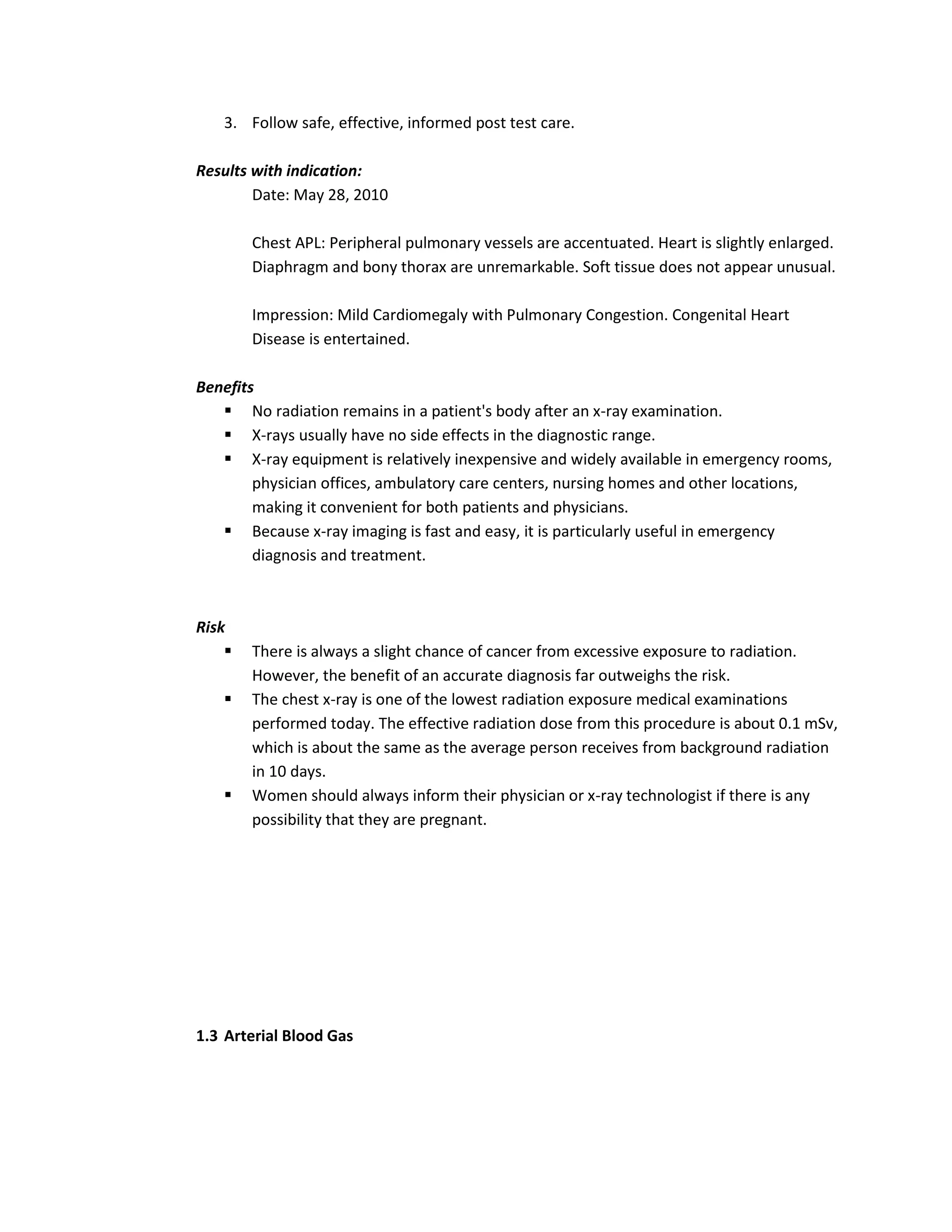
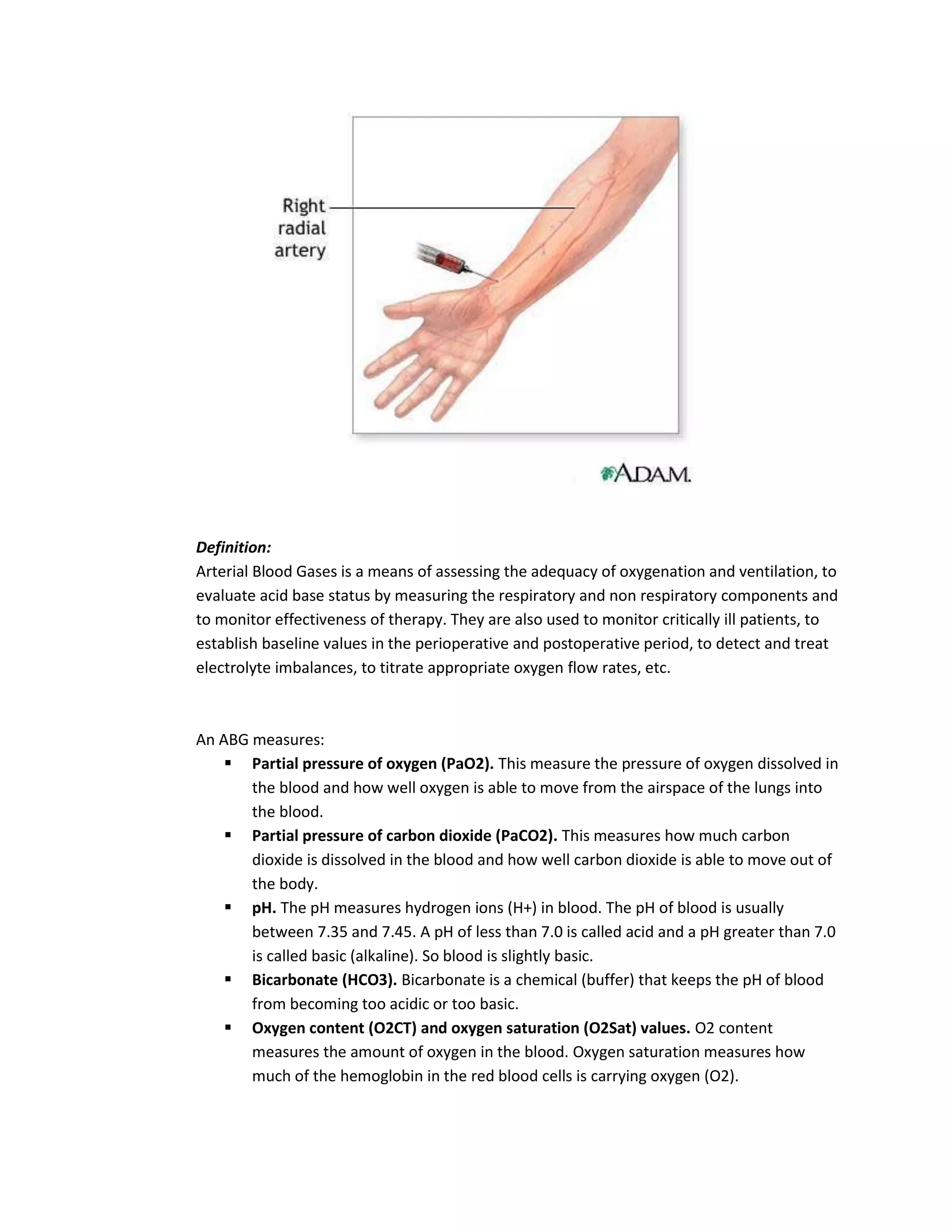
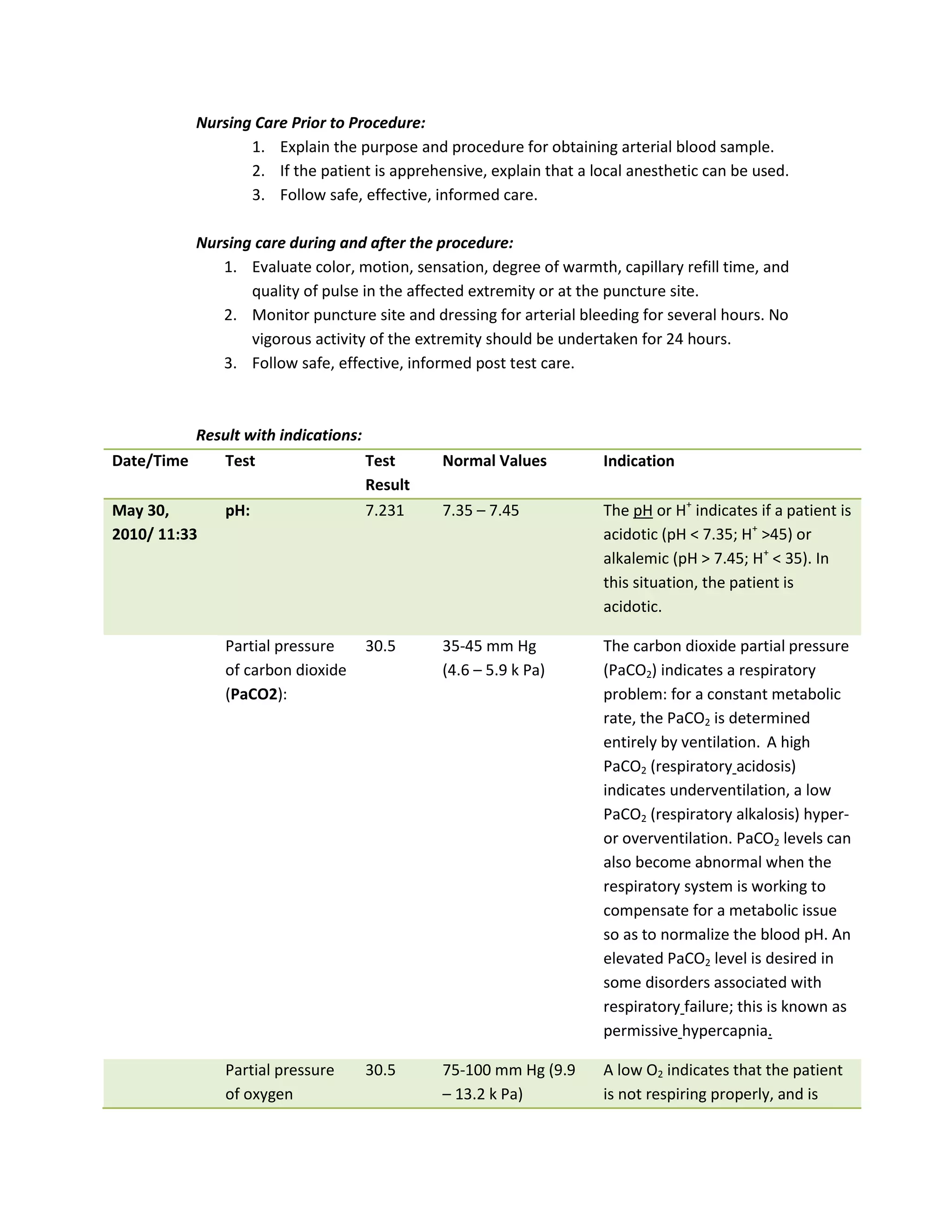
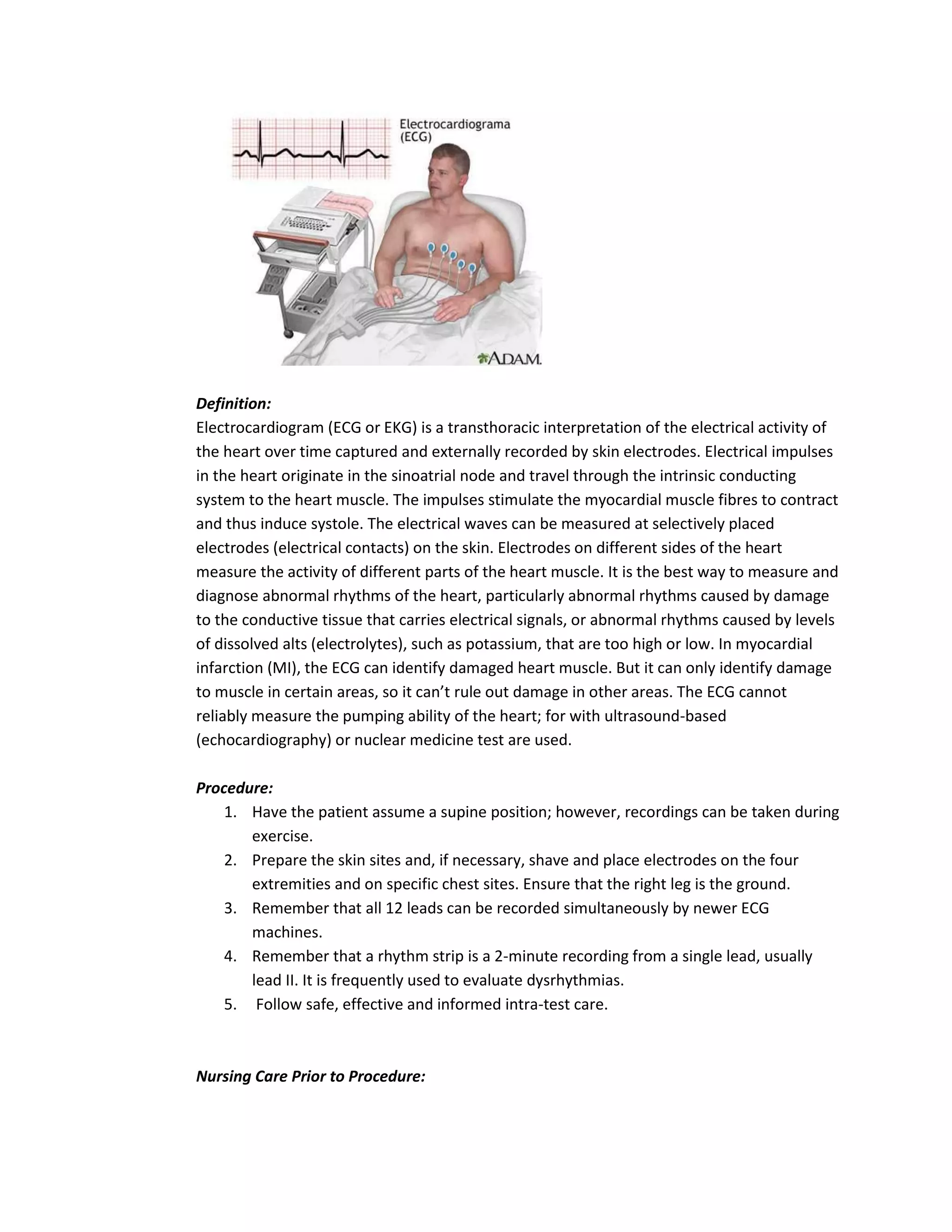
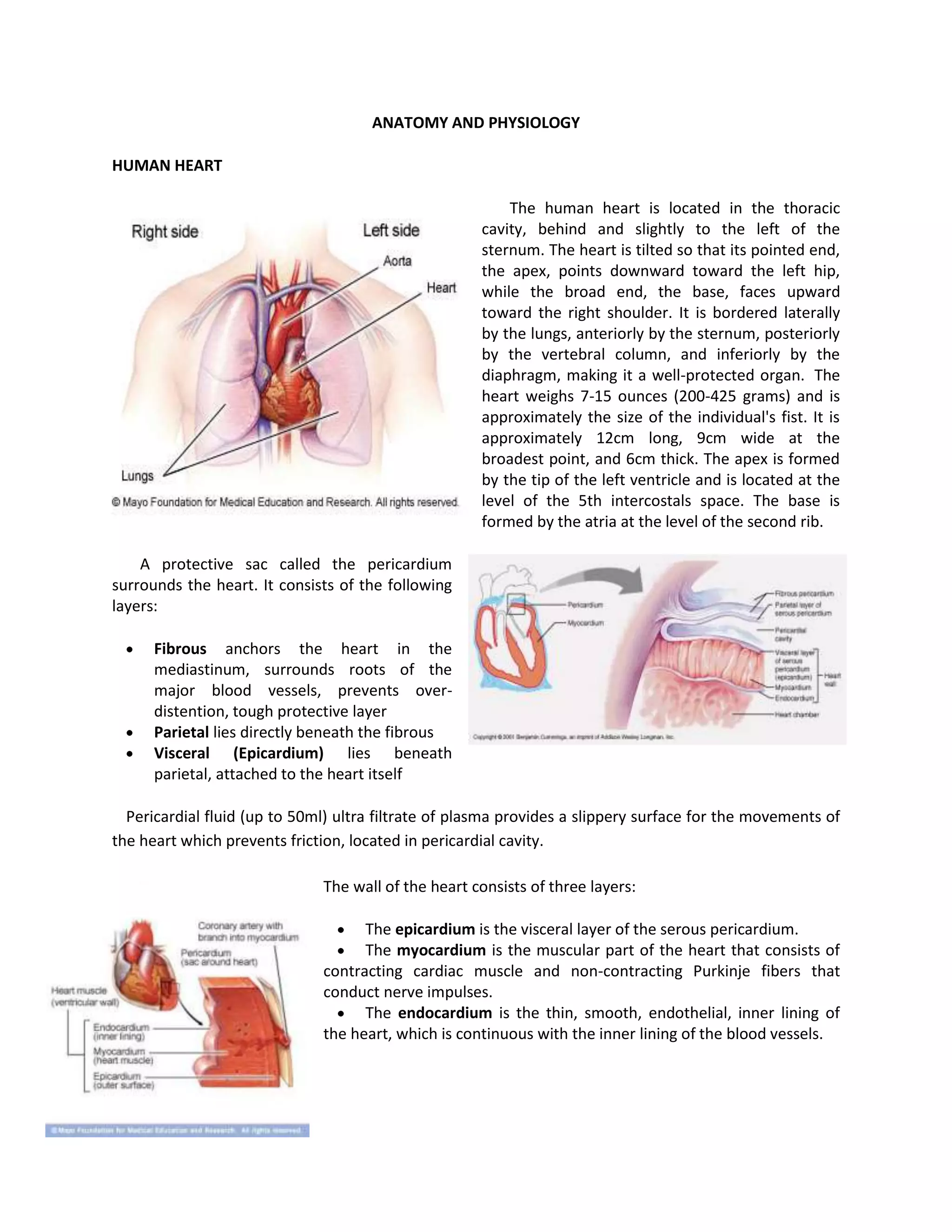
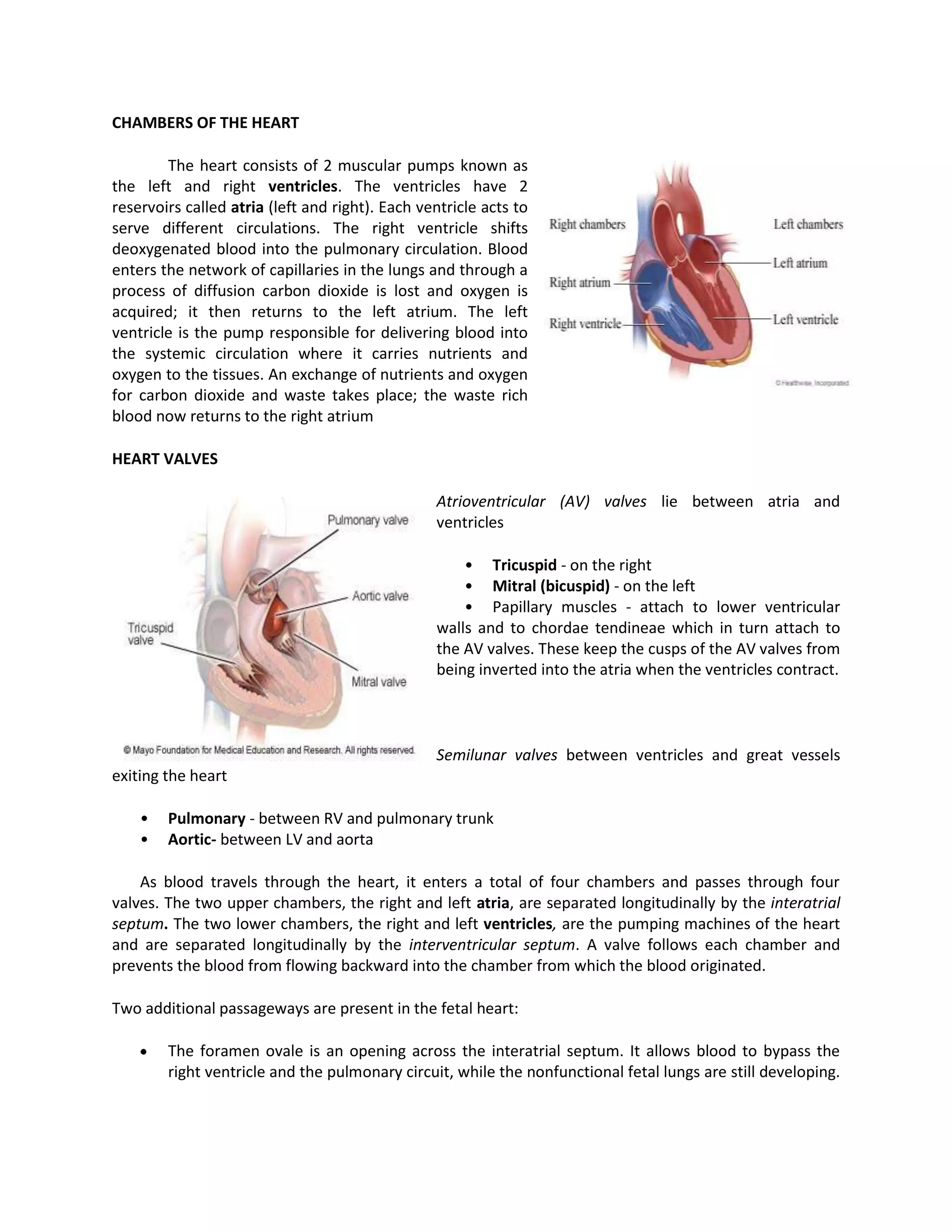
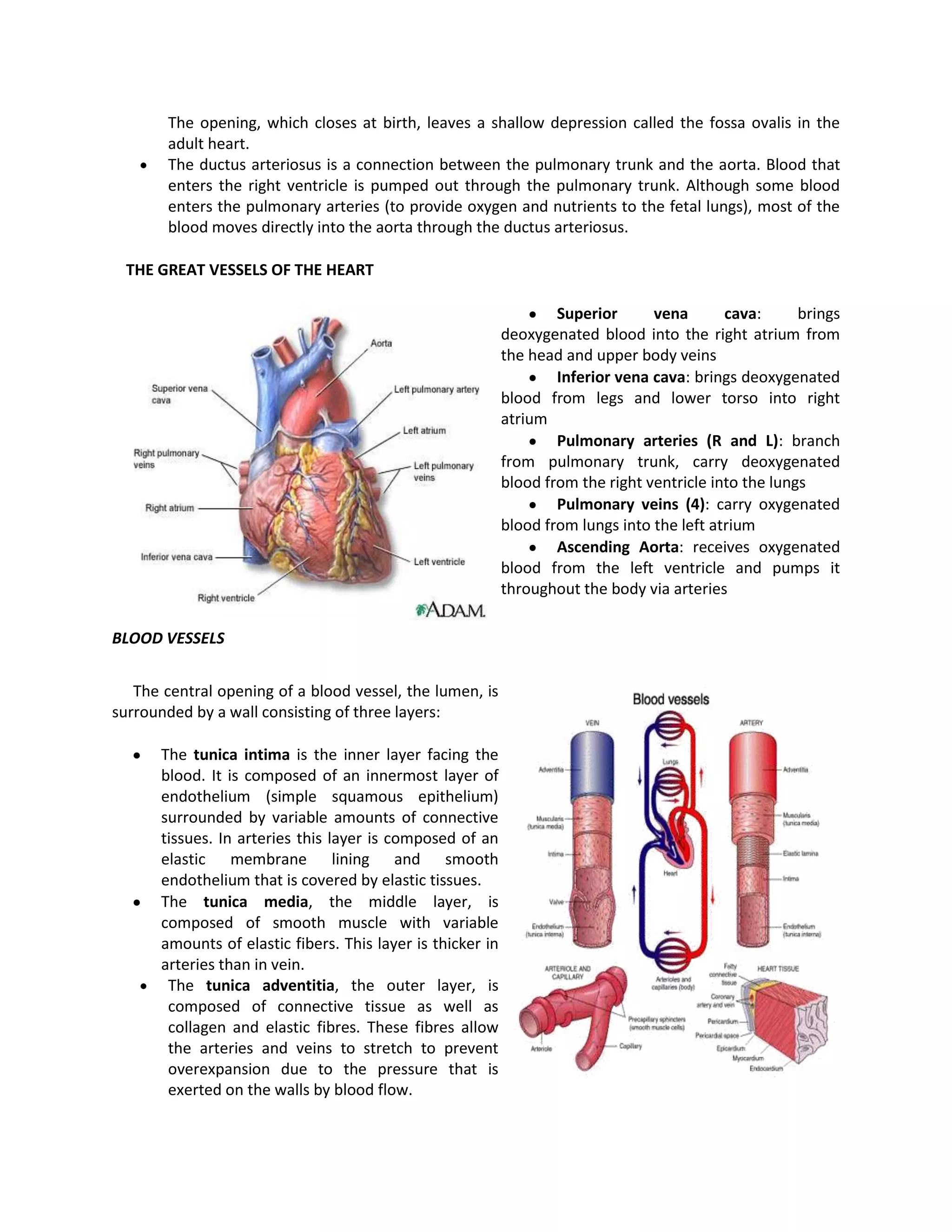
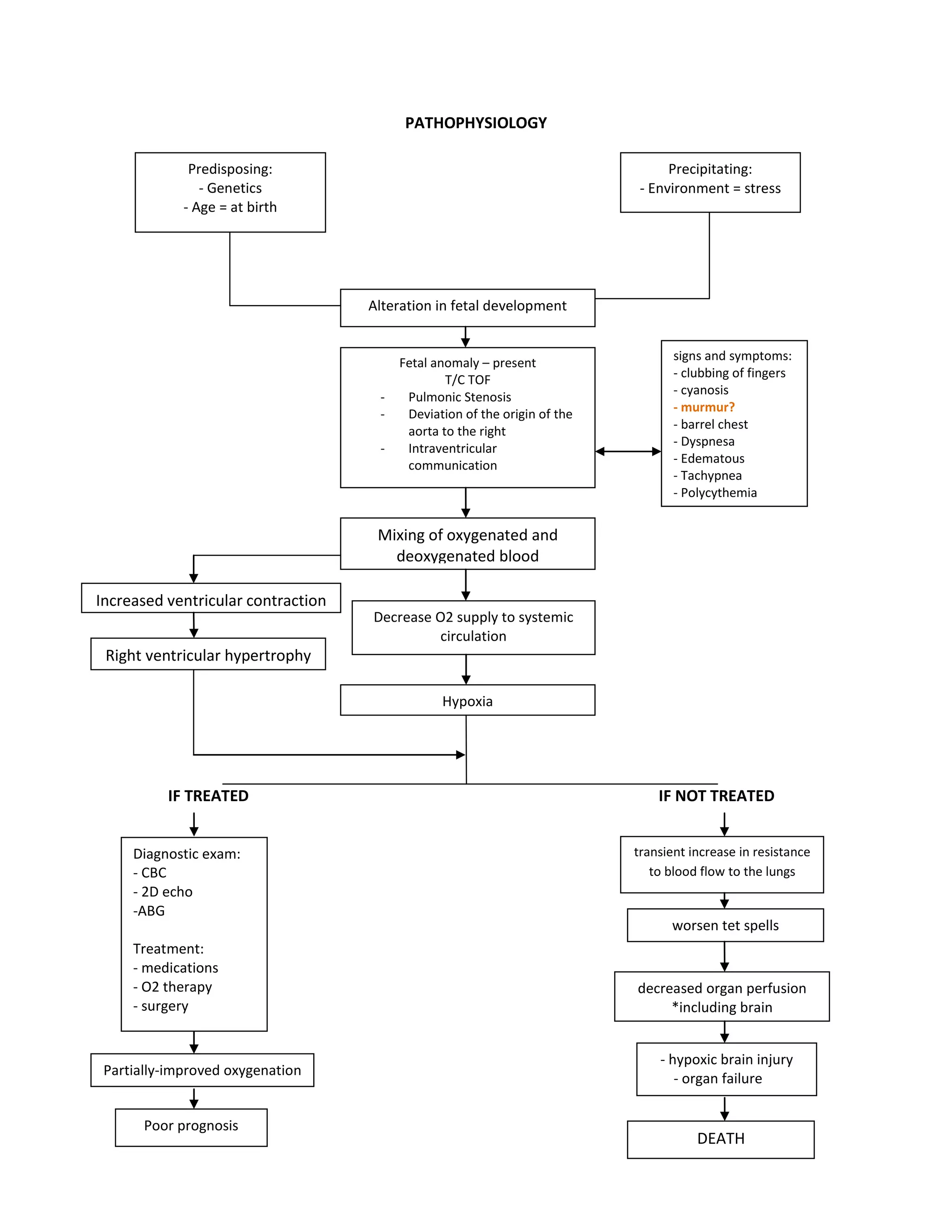
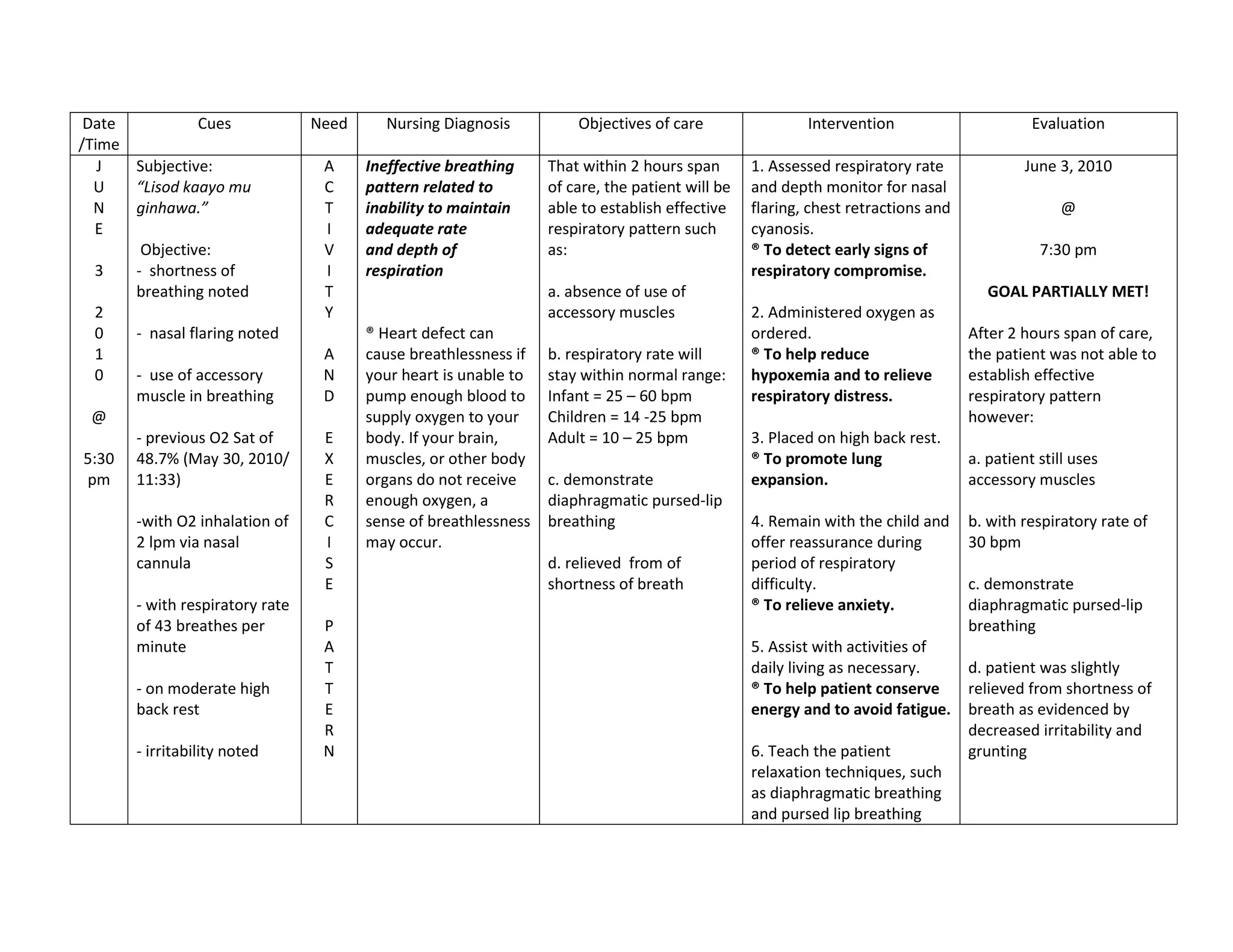
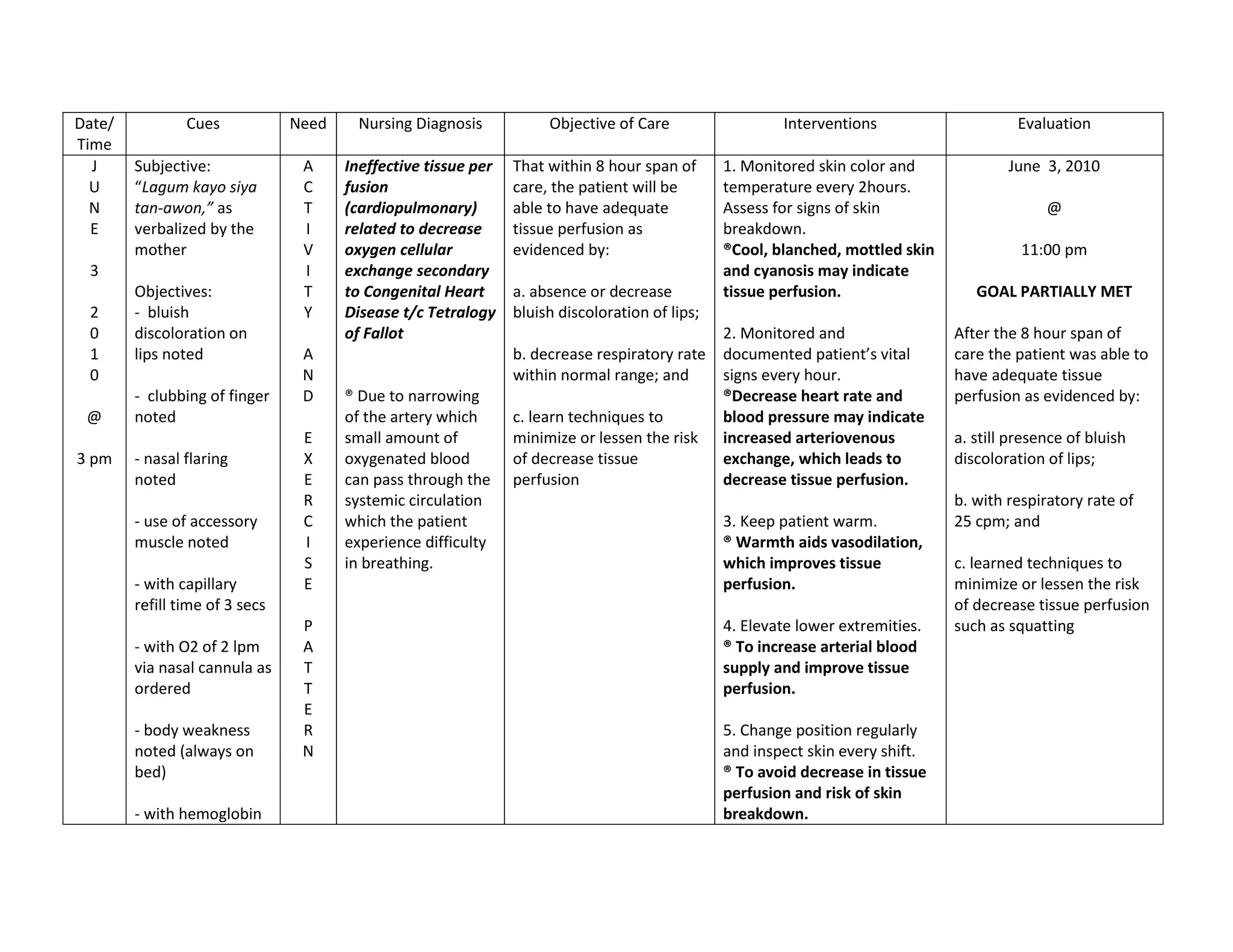
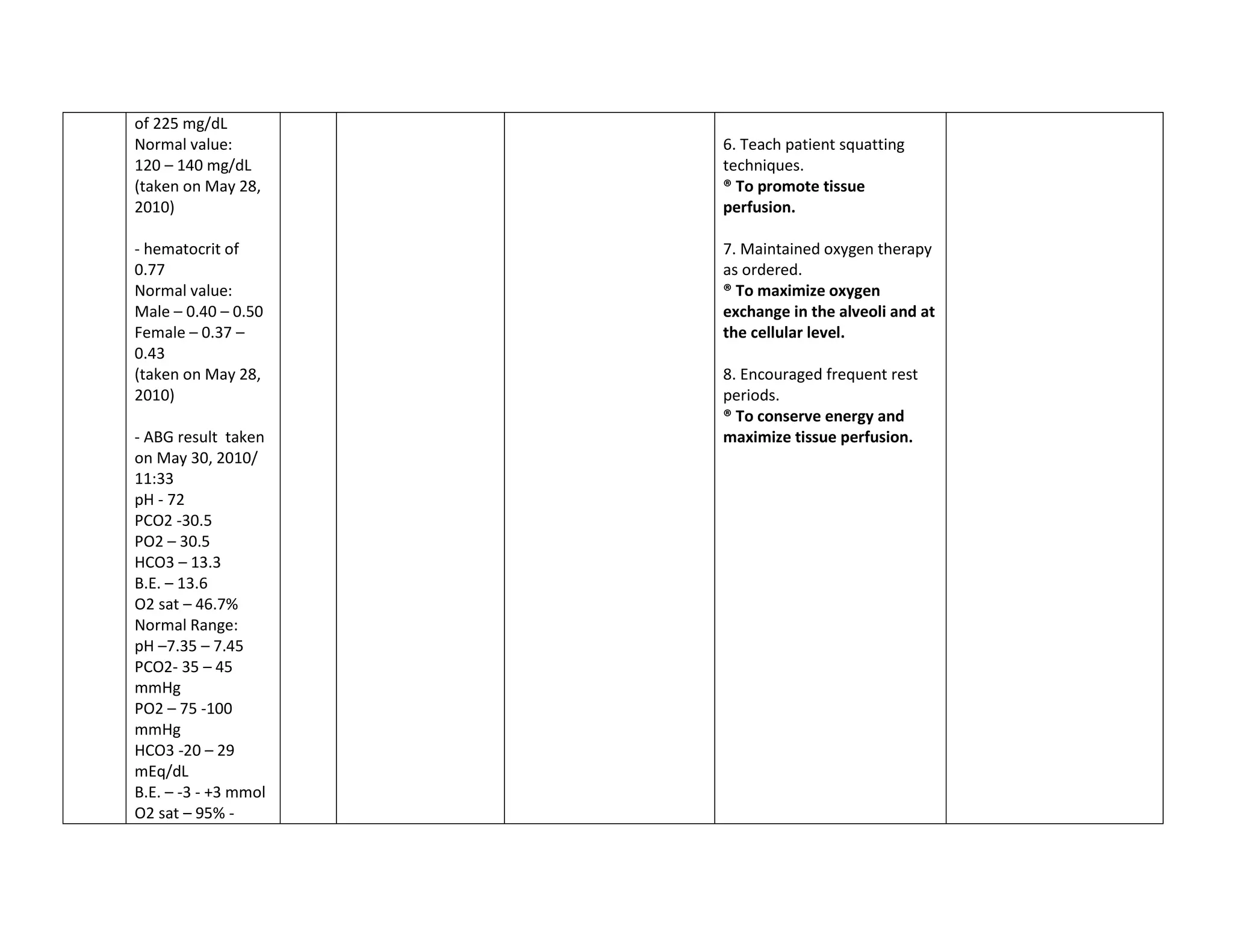
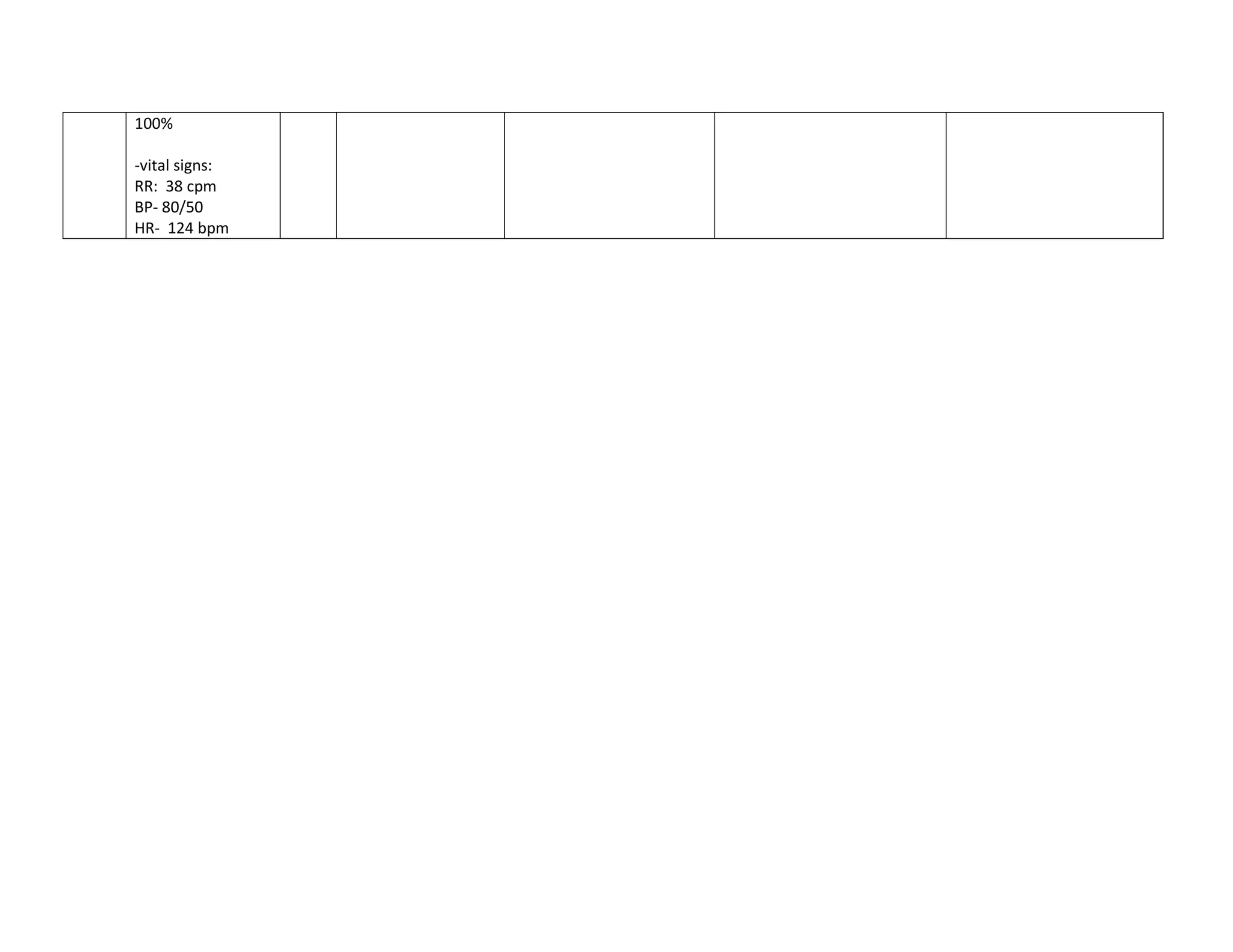
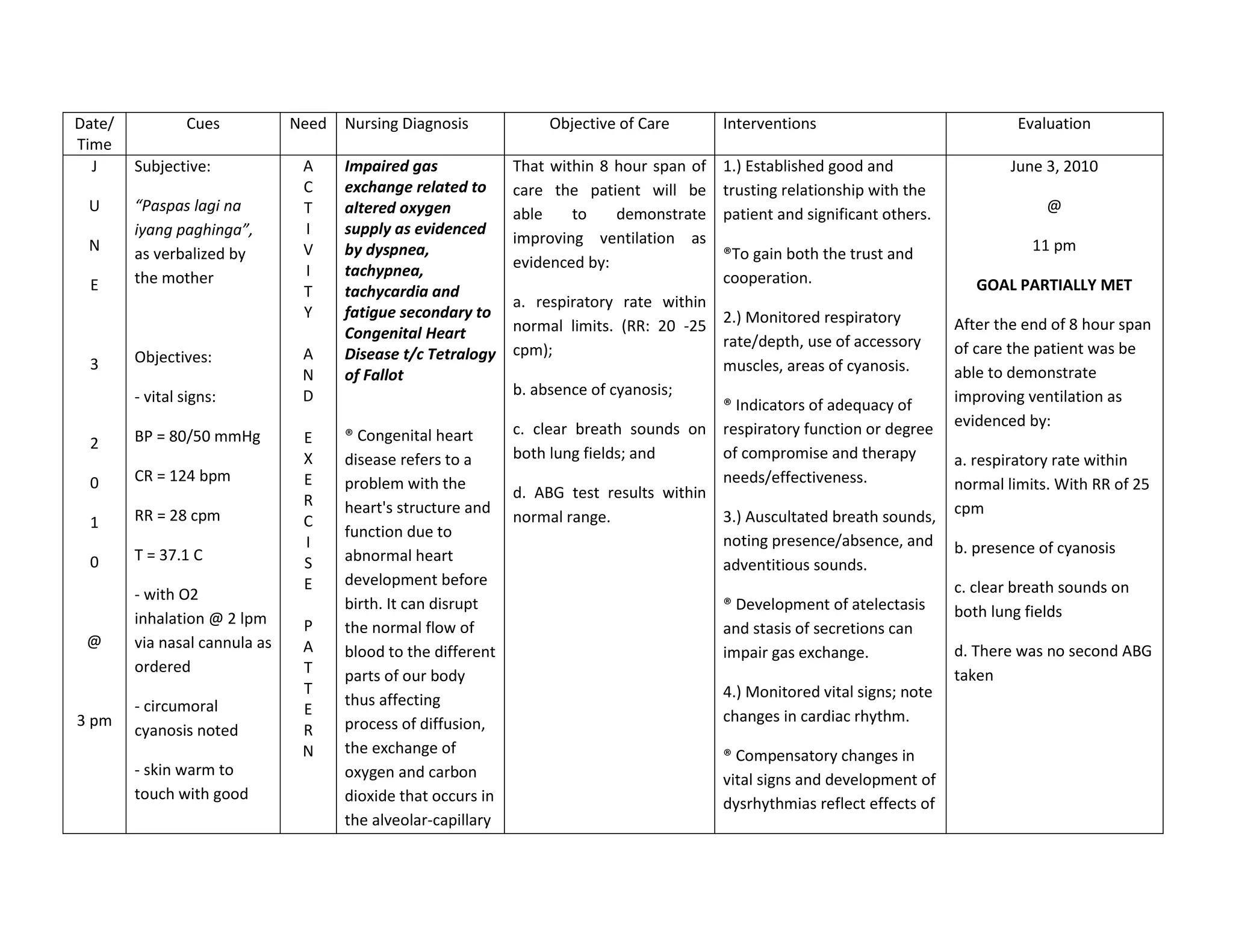
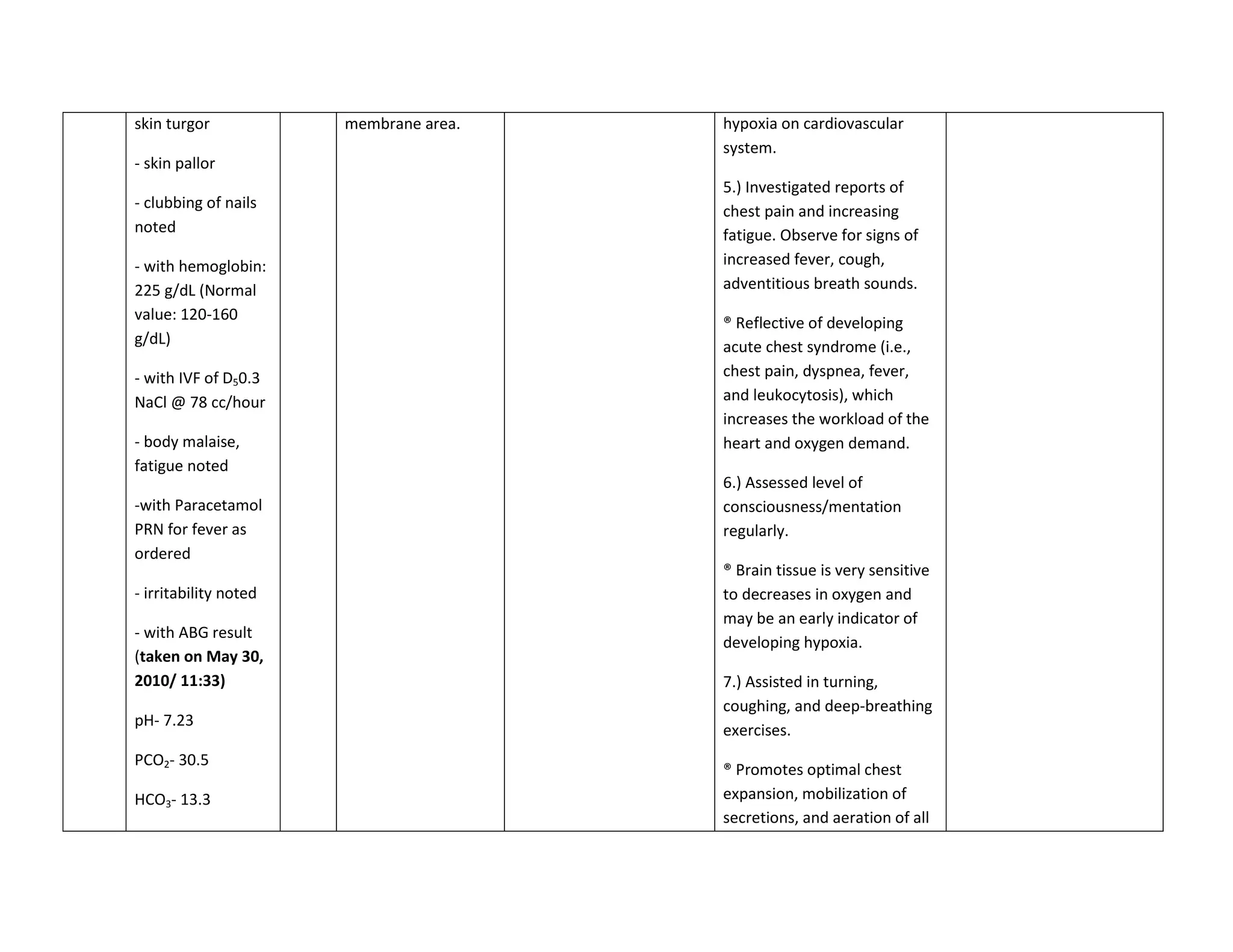
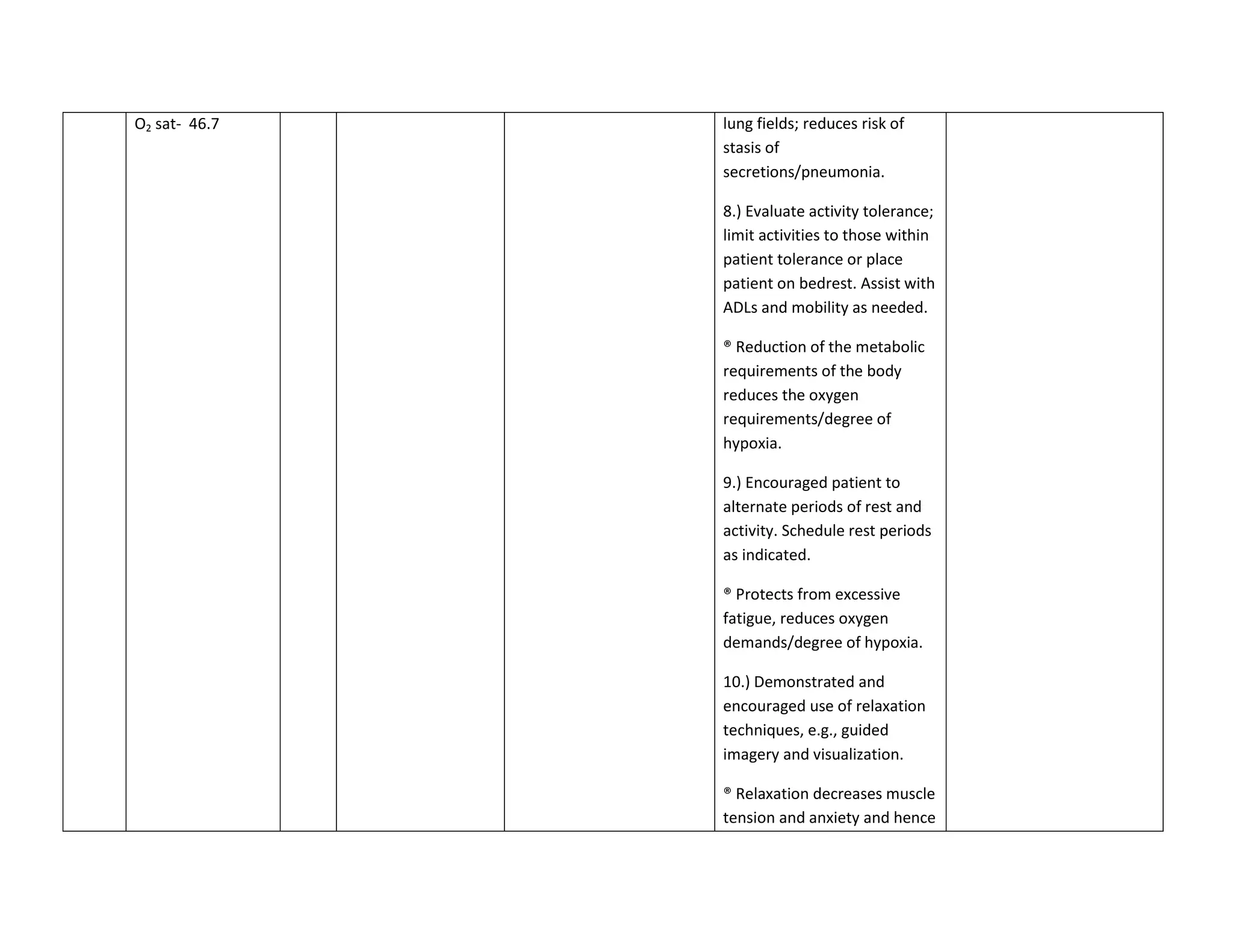
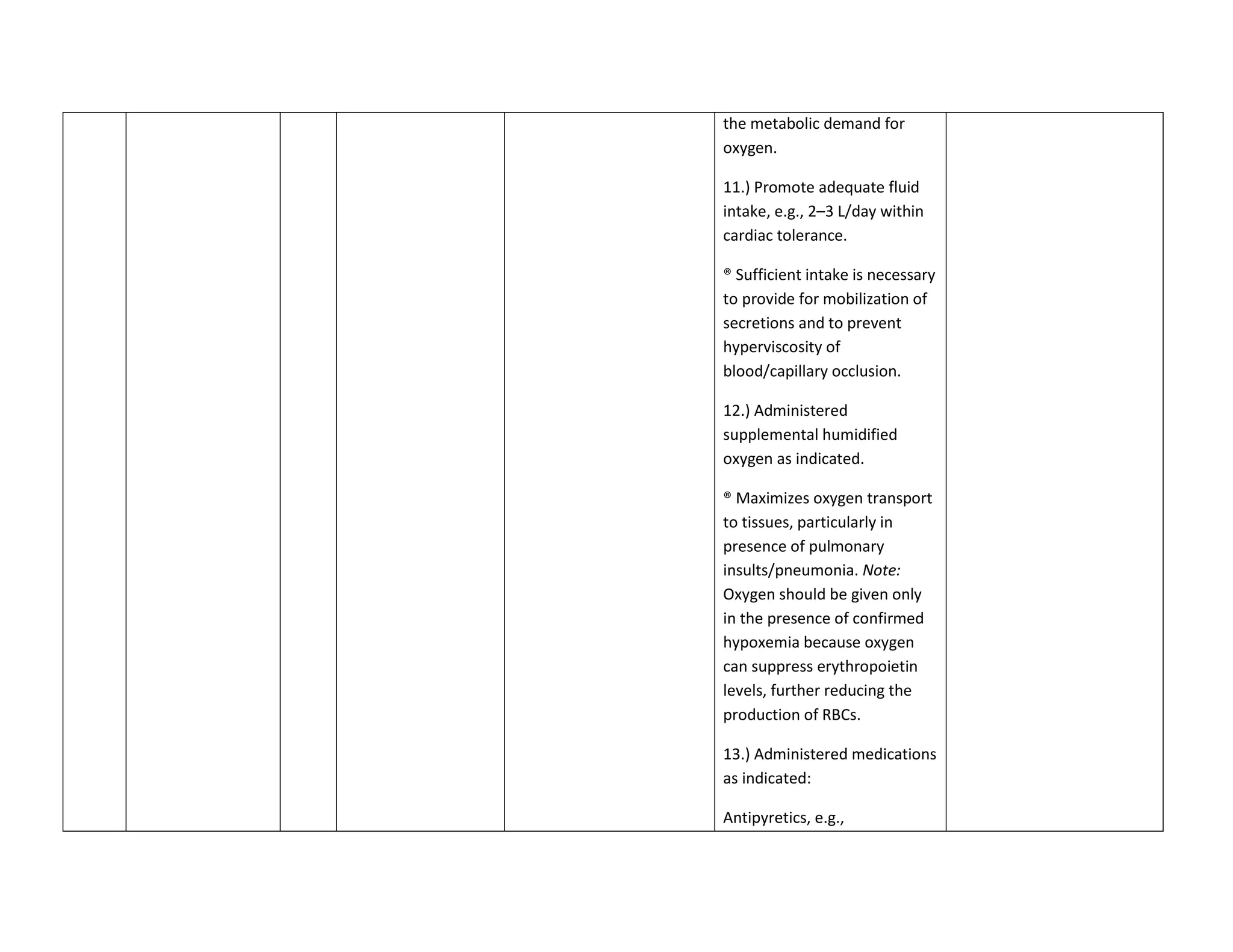
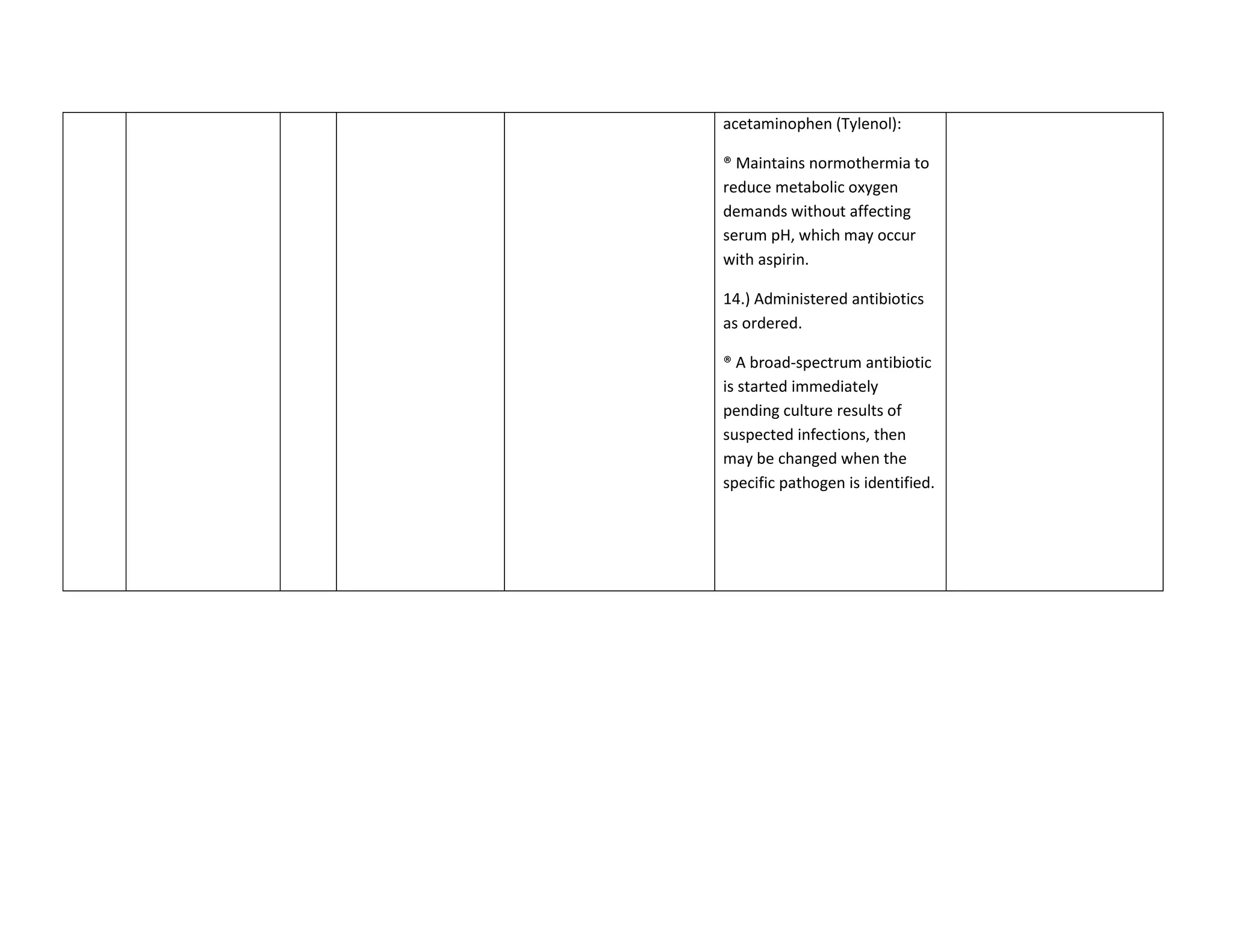
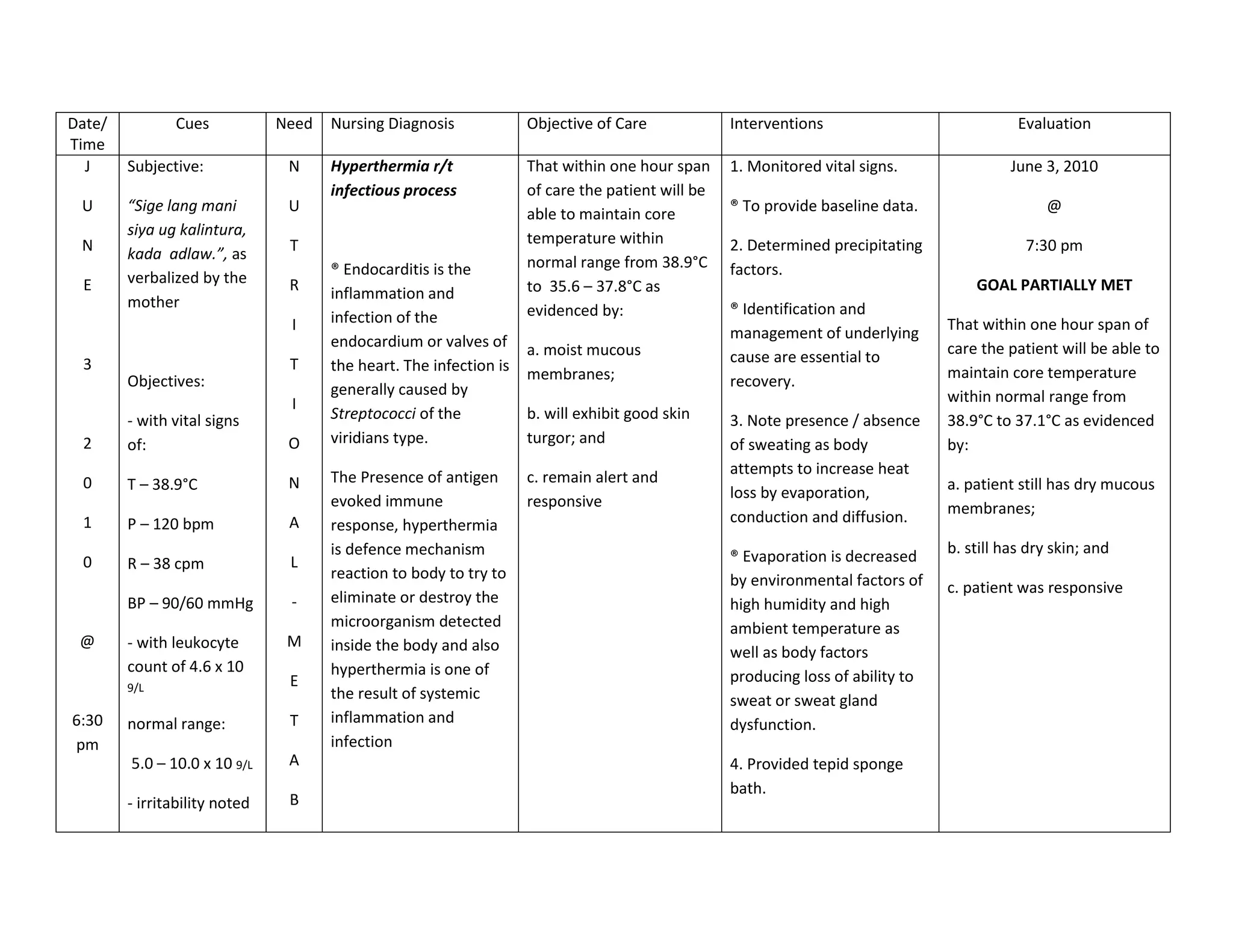
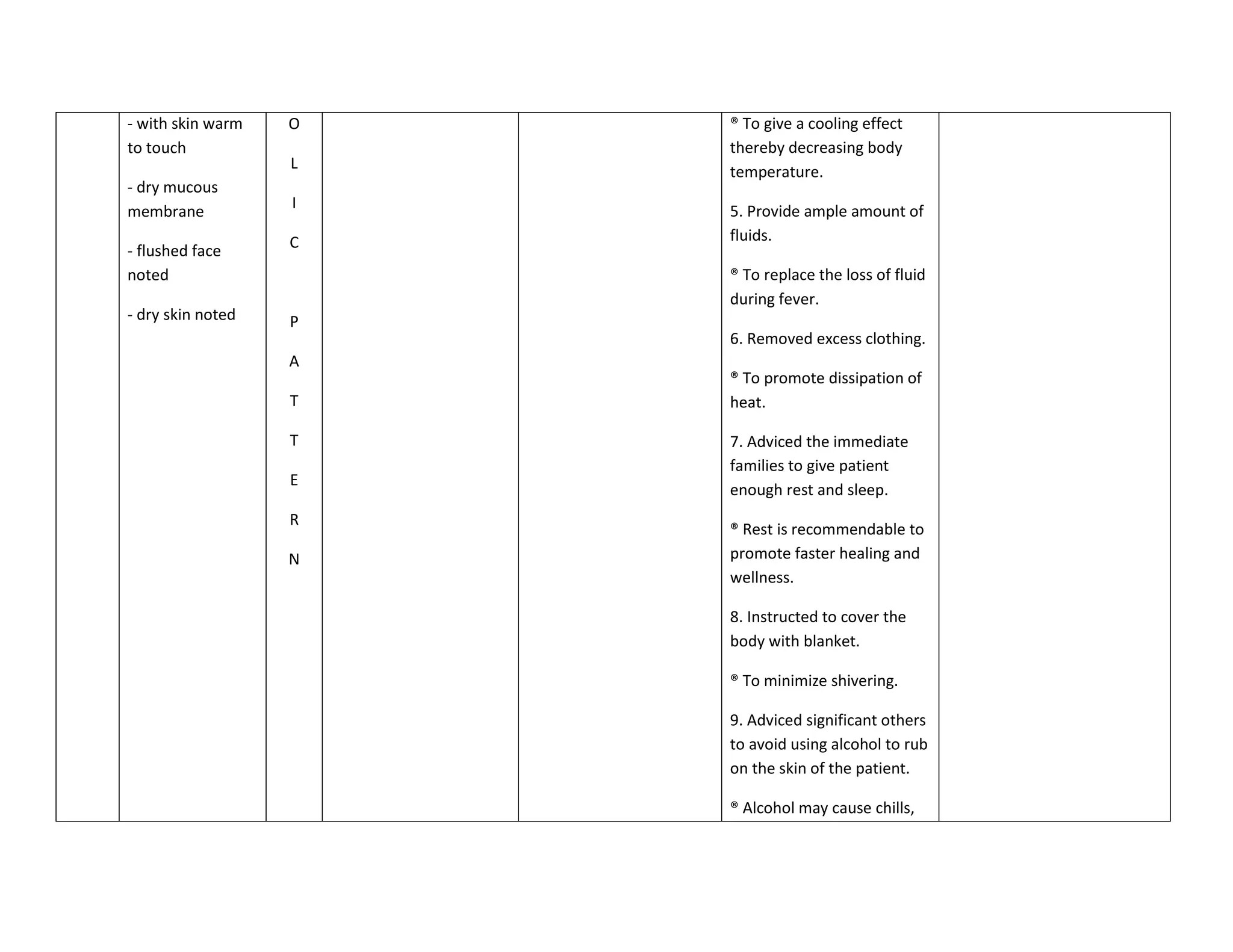
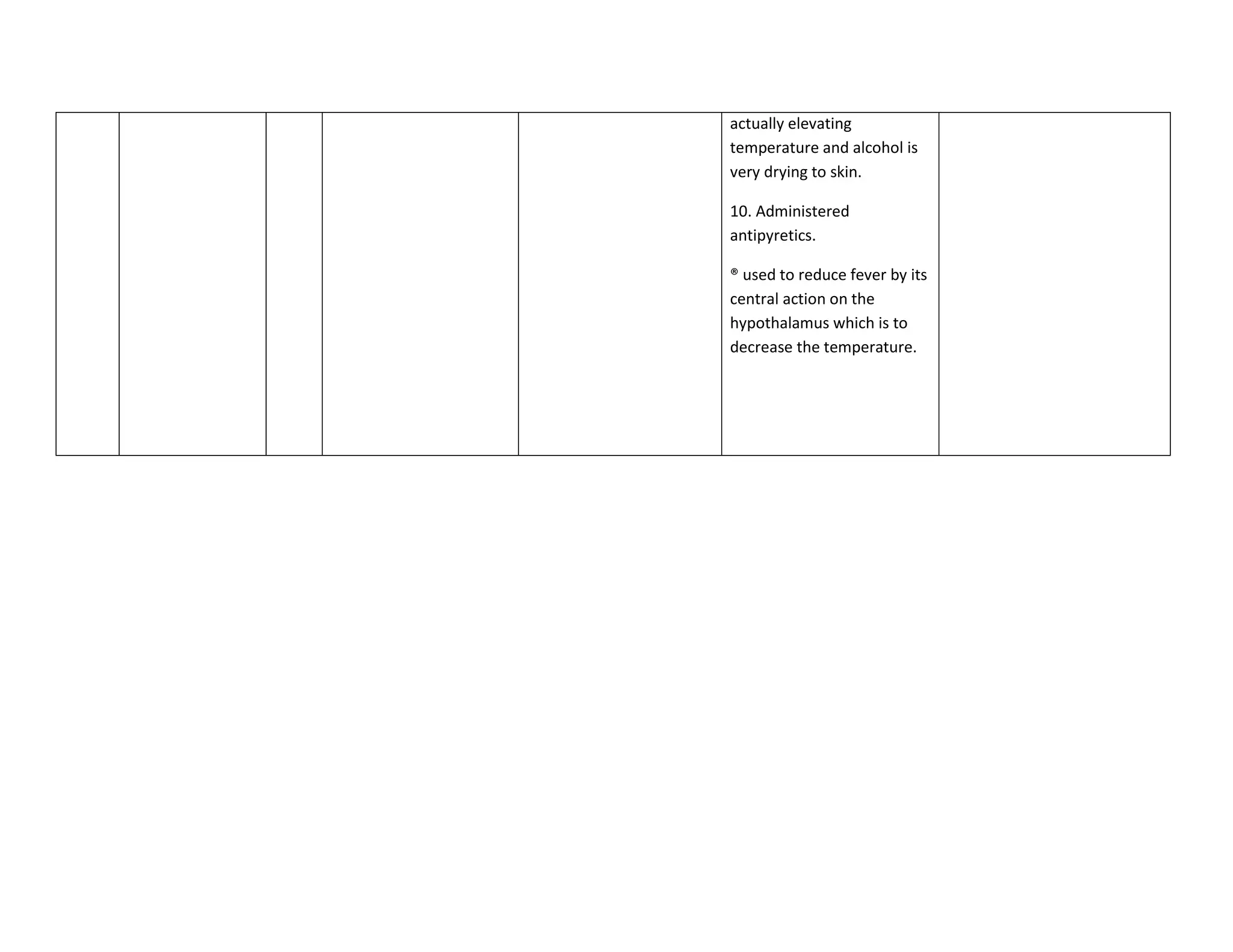
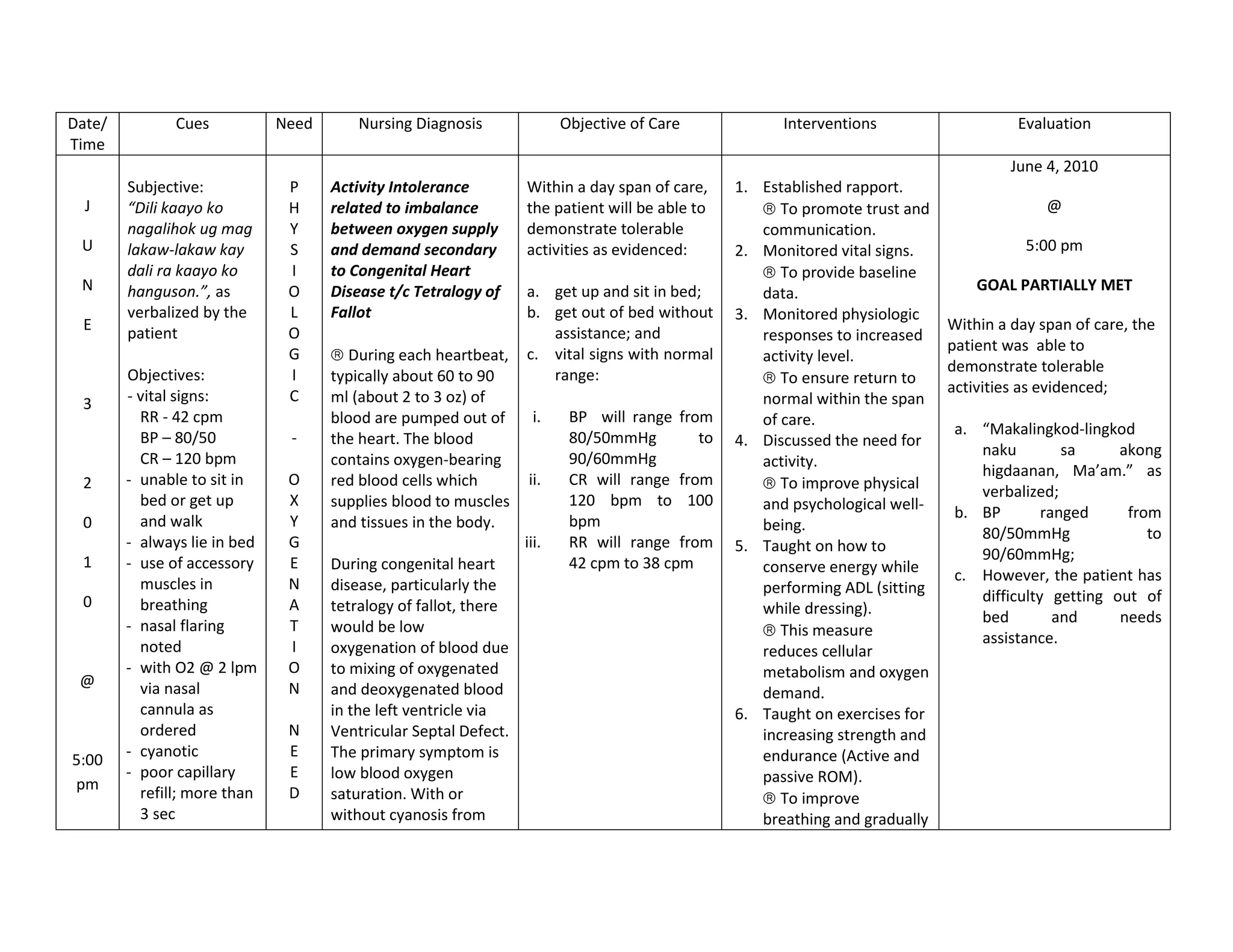
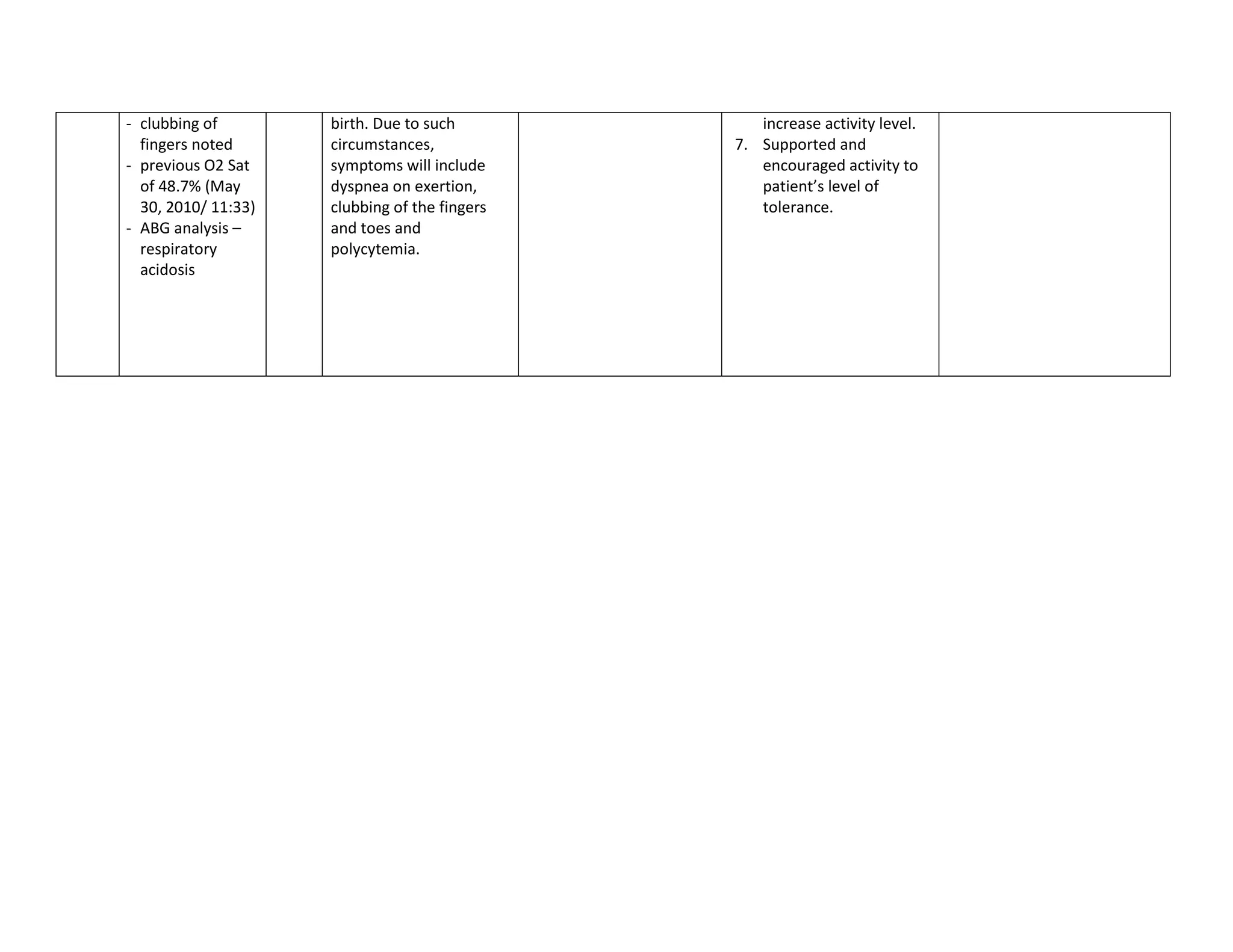
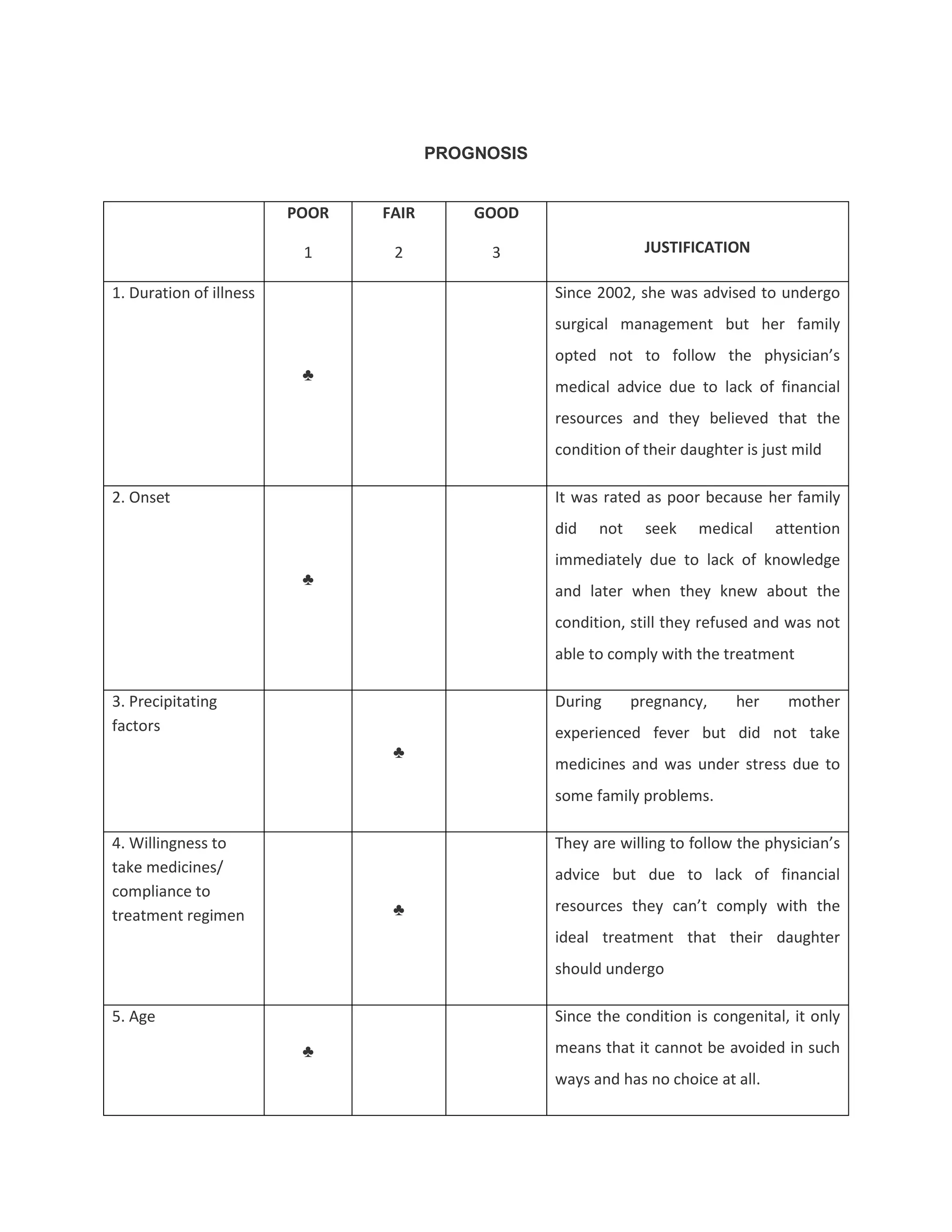
This document discusses congenital heart disease, specifically focusing on a 9-year-old female patient diagnosed with tetralogy of Fallot, a cyanotic congenital heart defect. It details the patient's medical history, current condition, and ongoing diagnostic work-ups, including nursing care and treatment plan considerations. The document aims to educate healthcare professionals on managing such cases and emphasizes the importance of family support and self-reliance in patient health management.