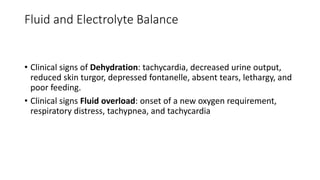
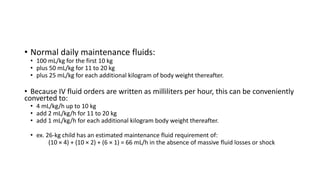
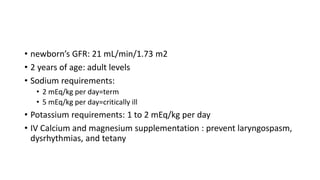
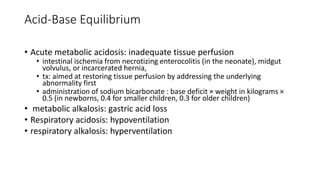
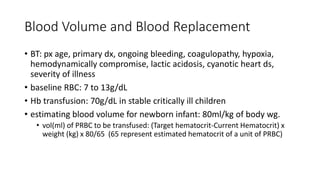
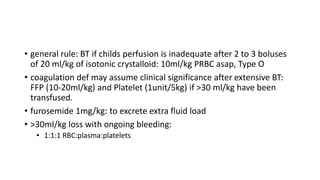
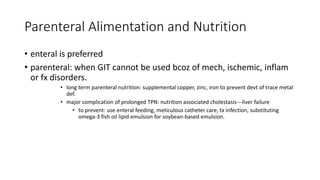
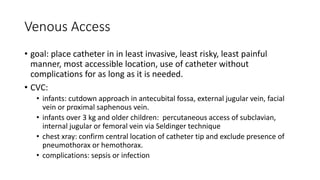
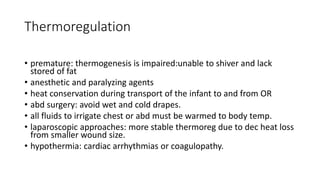
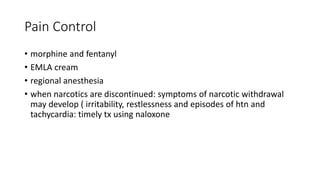
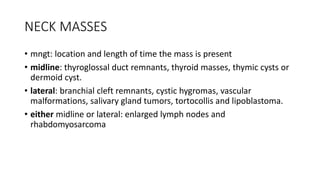
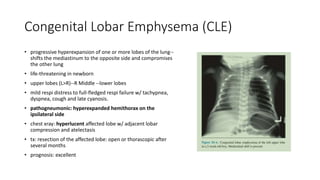
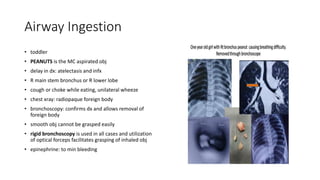
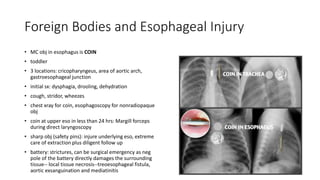
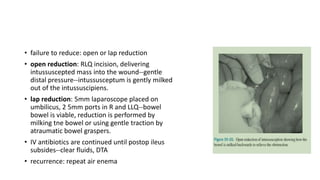
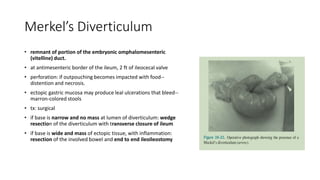
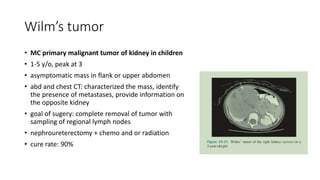
The document discusses key aspects of pediatric surgery, emphasizing that children are not simply smaller adults and have unique medical needs. It covers essential considerations in fluid balance, post-operative care, pain management, and surgical techniques for various pediatric conditions such as congenital disorders and airway obstructions. The guidelines provided also address the management of complications, nutritional needs, and the importance of careful assessment in treating pediatric patients.