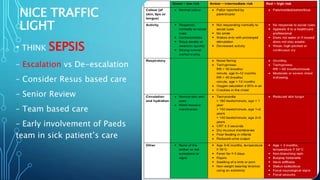
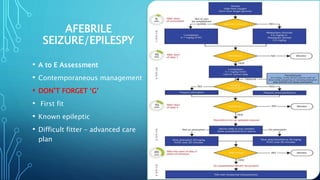
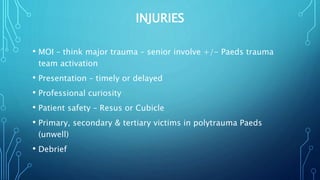
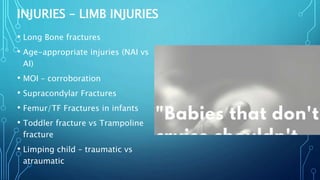
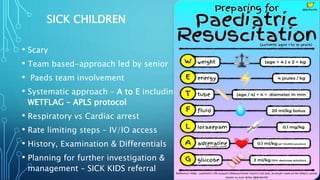
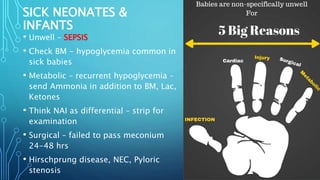
This document provides guidance on approaching and managing common pediatric emergencies. It emphasizes taking an age-appropriate approach, thorough history and examination, involving pediatric nurses and specialists as needed, following guidelines like NICE, and considering rare or serious diagnoses. Common presentations like fever, wheezing, injuries and seizures are discussed. The importance of senior review, ongoing assessment, and team-based care for sick children is stressed.

![FEVER
• URTI (including Tonsillitis) &/or EAR INFECTION – Abx or no
Abx
• Chest Infection – CXR or no CXR
• UTI – Culture or no Culture; Abx or no Abx
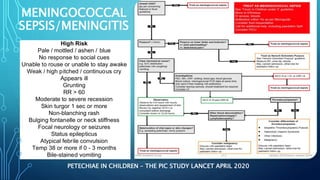
• Meningitis/Meningococcal Sepsis/Encephalitis
• Septic arthritis, discitis
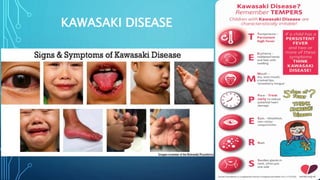
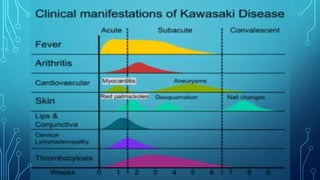
• ***KAWASAKI DISEASE
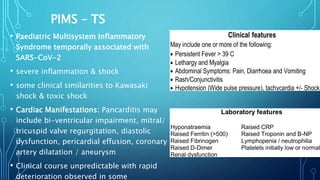
• ***PIMS-TS
Fever in under 5s: assessment and initial management
NICE guideline [NG143] Published: 07 November 2019](https://image.slidesharecdn.com/paediatricemergencies-211203110717/85/Paediatric-Emergencies-6-320.jpg)